The new Table of Contents on the left "or above in mobile" provides an easy way to navigate through each issue. However, we recommend scrolling through the entire publication when you first receive it to ensure you don’t miss anything. This is the Tennessee Nurses Association’s quarterly publication, and you’ll find all the same content in this digital format as before. We plan to implement changes as we progress, so your feedback is crucial in helping us improve the Tennessee Nurse. Please share your thoughts at kathryn.denton@tnurses.care.
The Tennessee Nurse
Table of Contents
Call for TNA Article Submissions
Submit an Article for Publication in the Tennessee Nurse
Article Submission Guidelines
TNF Silent Auction
TSU Receives Continuing Accreditation Through Fall 2031
Save the Date - Nurses Day on the Hill
American Nurses Association (ANA) Membership Assembly Update
A Message from ANA CEO, Angela Beddoe
A Lesson in Compassion
Microaggressions in Health Care – Part 1
TNF Pet Photo Contest
Healthcare Disparities within Hospice Care
Consumer Utilization of Technology in Healthcare: Exploring the Role of the Nurse
Part Of Your ANA/TNA Dues Is Tax Deductible!
Bridging the Generational Gap in Nursing: How to Foster Collaboration

September 2024
Fall Quarterly Newsletter
TNA Introduces a Fresh Digital Format for the Tennessee Nurse
I AM TNA
 Laura Barry, MSN, RN, CEN, TCRN
Laura Barry, MSN, RN, CEN, TCRN

My name is Laura Barry, and I am a member of District 2 of the Tennessee Nurses Association. I was raised on a tobacco farm in East Tennessee with strong Appalachian roots. My mother and grandmother are Appalachian women known for resiliency, a strong work ethic, and pragmatism. Appalachian women fight for their families and beliefs unapologetically. I decided to become a nurse in a similarly pragmatic way—I wanted to be able to provide for a family. I applied to every state school that had a nursing program and picked the school that gave me the best scholarships, the University of Tennessee at Chattanooga.
While I did not have an idealistic reason for becoming a nurse, after I graduated and became an emergency nurse, I realized that nursing is so much more than a paycheck. I was twenty-one years old when I took my first patient assignment. As a night shift emergency nurse, I got to see the best and worst of humanity. Babies were born to proud mothers, and people died too young. Nursing taught me that life and death are intimately linked and that I still had much left to learn about what it means to be a human. Nursing has been both a tragic and a beautiful teacher, one whose lessons never cease.
Through my experience at the bedside, I witnessed firsthand the systemic disempowerment of nurses. We are entrusted to be the hands of healthcare, but our voices are often ignored about ways to improve the system. I wanted a louder voice and the power to make a more widespread impact. I sought a master’s in nursing education to give my voice that volume, which led me to a nursing education preceptorship at the University of Tennessee, Knoxville (UTK).
Joining TNA
TNA District 2 hosts Healthcare Policy Day every year, at which Dr. Carole Myers speaks to area nurses and nursing students about the legislative actions that the Tennessee Nurses Association (TNA) is currently pursuing. I attended Healthcare Policy Day during my preceptorship at UTK in February 2020. Hearing about the way that TNA advocates for the disempowered through the legislative process inspired me to add my voice to this passionate group of nurses. That night, I went home and joined TNA. Though I have only been a member of TNA and the American NursesAssociation (ANA) since 2020, those memberships have afforded me countless experiences to demonstrate that nurses arepowerful. We can drive healthcare and healthcare policy if we unite our voices to advocate for our patients and profession.
Why it Matters?
Today, I am an instructor at the University of Tennessee, Knoxville, and continue to work as a bedside emergency nurse. I try to impart upon my students what was taught to me through my Appalachian familial culture. I want my students to know they can and should fight for their beliefs. I believe in fiercely advocating for the disempowered within the Tennessee healthcare landscape. I love being a part of TNA because I can see the actions of this group of nurses and the impact those actions have on healthcare within our state. I am the secretary for District 2 and have had the opportunity to see and meet the incredible nurse leaders within this state. I believe that healthcare is far from perfect and that nurses have the insight needed to enact change, but only if we are willing to work together. By working beside other nurses, TNA helps give me a voice, and that gives me optimism for the future.
From the President
 Ray Coe, PhD, MBA, MHA, RN-BC, NEA-BC, FACHE(R)
Ray Coe, PhD, MBA, MHA, RN-BC, NEA-BC, FACHE(R)

Recently I heard an individual express their frustration that since an organization would not speak for them, they felt their voice was being silenced. As long as you have a voice, as long as you can write, you cannot be silenced! You may not have the platform you desire, but you are not silenced! You have the option of writing letters to the editor, articles, or social media posts. You may speak at public meetings or buy time on public airways, but you are not silenced!
For example, currently, America is in the middle of a Presidential election, as well as many other federal, state, and local elections. You have the right to endorse a specific candidate or ballot initiative and ask others to vote for your choice. However, you should back up your endorsement with facts regarding the candidate or ballot initiative. These facts may be obtained from public records or other sources that stand up to public scrutiny. Facts may lead to opinions, but opinions are not facts! Honestly, it is your assessment of the facts that led to your opinion and your endorsement or support of a candidate or initiative.
But what facts should be considered? Consider information regarding thought, word, and deed. Regarding thought, consider what the candidate says they will do or what supporters of the candidate or initiative say will happen if elected. What are the candidate’s reasons for running, or why was the initiative proposed? This leads to words: what has the candidate or supporters of the candidate or initiative said? What is the goal of the candidate or initiative as stated by the candidate or by the wording of the initiative?
Finally, what is the history of the candidate or supporters of the initiative? What deeds have they, and the people with which they surround themselves, done in the past, and are they in line with their current statements or goals? Carefully evaluate the facts and decide on a candidate or position regarding a ballot initiative, your assessment of the facts compared to your goals and values, and make an endorsement.
You have a right to make your endorsement, to donate to your chosen candidate or initiative position and to make your endorsement public. But this does not mean that others must agree with you. They have the right to go through the same decision-making process and make a different decision.
You may have a public debate about the facts or decision-making process, but you should always remain civil and factual. Debate your facts and sources; explain your reasoning, but never insult the other person. Pick your battles and know when to walk away. However, remember - the most important thing you can do for your choice is vote!
From the Executive Director
 Kirk W. Lawson, CAE
Kirk W. Lawson, CAE

Have you ever had one of those days when your mind feels like it’s playing the “Plinko” game from The Price is Right? Well, today, that is me. There is so much TNA news to share, I don’t know where to begin.
So, let’s start with Ray.
Ray Coe stepped into the President’s role last October and has been working hard to listen and take to heart the interests of all RNs in the State regardless of their membership status. He has also brought a renewed interest in collaborating and sharing resources with the American Nurses Association (ANA). To that end, he, along with board members Marilyn Smith, Courtney Nyange, and District 3 President Ashley Carter, collectively applied for a grant from ANA to support our efforts in advocating for a workforce that reflects the diversity of the communities nurses serve. TNA was awarded the grant, and as a result, we will have the opportunity to share the film Everybody’s Work: Healing What Hurts Us All, at our Annual Conference. Additionally, we will host a panel featuring ANA Past President Ernest Grant with facilitation by TNA members Ashley Carter and Courtney Nyange.
Our new Director of Operations, Marilyn Smith, has dedicated much of her time in her new role to reviewing TNA’s governing documents and helping to shape our future as a member of the Long Range PlanningCommittee. Marilyn’s work on updating our Mission Statement has been invaluable as we prepare to launch our new strategic framework at the Annual Conference.
Courtney Nyange, our new Director of Practice, has spent a great deal of time creating and recruiting members for a new Bedside Nurse Advisory Committee. I view this committee as vital to our future as we hope to bring the bedside nurse perspective to the forefront of our strategic initiatives.
Our new Government Affairs Director and chair of TNA’s GOVA committee, Mark Miller, hit the ground running as well. Mark has held listening sessions with every active TNA District in an effort to learn about specific issues that most affect each District and nurse in the State. These sessions will directly impact our legislative agenda as we strategize for 2025 and beyond.
Christie Manasco, our Education Director and Primary Nurse Planner, has been one of the busiest and most productive board members of the past two years. In addition to her director responsibilities, she has worked closely with the South Carolina Nurses Association to ensure that TNA retains our status as an Approved Provider Unit which allows us to develop and offer nurse continuing education contact hours (CNEs) for TNA’s programs and events. Christie has also been collaborating with our newest partner, Whitecoat Technologies, in creating our new Virtual Continuing Education platform which will launch this fall with a variety of CNE programs designed for both our nurse members and non-members.
Our Membership Director, Jennifer Hitt, continues her work in retaining TNA members at a time when membership organizations continue to struggle. She, along with Christie, created the re-imagined Nurse Educator Institute (NEI), which TNA has presented twice in the past two years. The NEI is a program designed to help new and current Nursing School Faculty members succeed in their role as nurse educators. This program was developed in partnership with and support of the Tennessee Deans & Directors of Schools of Nursing.
We are pleased to partner with the Tennessee Hospital Association (THA) in support of the Belmont Inman College of Nursing for Innovation Summit 2024. As part of the Summit, TNA President Ray Coe and TNF’s new President, Loretta Bond, revealed our new Innovation Grant Program. The initial funding for the program is being underwritten by the Tennessee Nurses Foundation, as they have set aside $25,000 to fund our first grants.
That brings us to our Annual Conference: Transforming Nursing Together, which will take place on October 10-12 at the Hilton Garden Inn in Mt. Juliet, Tennessee. This year’s conference will be filled with exciting speakers and networking opportunities, not to mention our exhibitors and poster presenters who always bring their “A” game to our conference.
The conference will feature topics as diverse as jazzing up micro-learning to better understand the journey of internationally educated nurses, nursing innovation to compassion fatigue, research and evidence-based practice to assessment in domestic & intimate partner violence, the era of open notes to micro-aggressions, building resilience in undergraduate nursing students to understanding the attitudes and perceptions related to full practice authority, conflict management to transactional to transformational.
TNA will conduct the business of the association at the Membership Assembly during the conference, and once again this year, every TNA member will have the opportunity to vote during TNA’s annual election of officers, directors, and nominating committee members. More details on this will come later. In the meantime, check out the Slate of Candidates and view each candidate’s video HERE.
The Tennessee Nurses PAC (TNPAC) is planning an old-fashioned Ice Cream Social, and we can’t forget the Foundation’s auction and wine pull. There is something for everyone at this year’s conference; you don’t want to suffer from FOMO. To register for this year’s conference, click here.
I’d say TNA's “Plinko” puck is definitely headed for the winner's slot.
Call for TNA Article Submissions
Submit an Article for Publication in the Tennessee Nurse
Article Submission Guidelines
General Topics: any topic related to nursing will be considered for publication. However, articles that speak to the broad scope of nursing are preferred rather than a narrow audience.
Nursing Research: Nursing research project submissions are welcomed.
In Each Issue--Topics related to each of the below specific sections
- I AM TNA
- Spotlight on Practice
- Spotlight on Nursing Fundamentals
- Nurses Well-Being
Articles and photos should be submitted by email to Kathryn.Denton@TNurses.Care. Submissions should be sent in Microsoft Word, titled, and with no headings or footers. Subheadings are encouraged for ease of reading. Please include two to three sentences of information about the author at the end of the article and list all references. References are sometimes not printed but are available upon request.
TNA is not responsible for unsolicited freelance manuscripts or photographs.
Although authors are not required to be members of the Tennessee Nurses Association, when space is limited, preference will be given to TNA members. If you have questions, please contact Kathryn Denton, Managing Editor, at 615-254-0350 ext. 3 or email Kathryn.Denton@TNurses.Care
The Tennessee Nurse—Official Publication of the Tennessee Nurses Association
Spotlight on Practice
Alternatives to Opioids for Chronic Pain
 Charlotte Chavous, BSN, RN, AMB-BC, CHT
Charlotte Chavous, BSN, RN, AMB-BC, CHT
 Amber Lauer, MSN, APRN, FNP-BC, CHT
Amber Lauer, MSN, APRN, FNP-BC, CHT
 Debra Rose Wilson, PhD, MSN, RN, AHN-BC, CHT, SGAHN
Debra Rose Wilson, PhD, MSN, RN, AHN-BC, CHT, SGAHN
Alternatives to Opioids for Chronic Pain
The United States is currently wading through an opioid epidemic. The CDC reports that 75% of drug overdoses involve opioids, and the number of deaths has increased over 6 times between 1999 and 2021 (CDC, 2023). The overdose rate increased by 30% during COVID-19, from 2019 to 2020 (mostly fentanyl), and those who have substance abuse disorders had a higher risk for poor COVID-19 outcomes (NIDA, 2023). Chronic pain is reported to have a yearly economic cost of over 600 billion dollars in the United States and affects more than 100 million Americans. Opioids are a poor choice for chronic pain. As nurses, we see the outcomes of substance misuse, but we also see a need to offer other evidence-based ways to help manage pain for our patients. Numerous other effective, evidence-based modalities can give patients tools to better manage their pain and have an increased quality of life. In the dynamic realm of healthcare, nurses continually seek innovative approaches to ease the suffering of their patients. The patient needs an array of options, and a combination of any of the options may work best.
Types of Pain
Pain is classified as acute pain (sudden onset and lasts for a limited amount of time) or chronic pain (long-lasting and often resistant to medical treatment). There are more classifications, such as neuropathic pain, nociceptive pain, and radicular pain, and these are also often chronic. These subtypes are often chronic and may be intermittent or constant. Some examples of chronic pain are arthritis, fibromyalgia, or back injuries. In truth, pain is subjective. It is what the patient tells you it is. What helps one patient may not help another.
Guided Imagery
Guided imagery, also known as mental imagery in nursing care, is a therapeutic technique that involves using a nurse's guidance or recorded audio to help patients create and focus on mental images for specific therapeutic goals. It is a form of mind-body therapy that aims to harness the power of the mind to improve the patient's overall well-being and is used in mindfulness meditation to calm the mind. Nurses can help patients focus their attention on positive and calming mental images, diverting their minds away from pain sensations. This distraction can reduce the perception of pain and provide a sense of relief and comfort. The calmness empowers patients to play an active role in their pain management, fostering a sense of control and self-efficacy. The five types of guided imagery in nursing care not only complements traditional pain management methods but also supports holistic and patient-centered approaches to healthcare.
Sensory-focused imagery encourages patients to vividly imagine soothing sensations, such as warmth, coolness, or gentle touch. Nature imagery, including picturing serene landscapes or tranquil natural settings, can promote relaxation and distract patients from their pain. It has the power to transport patients to a calmer mental space. Healing imagery involves patients envisioning their bodies healing and regenerating. This idea can boost their confidence in the body's ability to recover and reduce anxiety related to pain. Positive affirmations, where patients repeat uplifting and empowering statements, can foster a more positive mindset and enhance their ability to cope with pain, ultimately reducing its impact. Patients can use symbolic images or metaphors to represent their pain and work through it mentally, transforming the pain into something more manageable or less intimidating.
Research shows that guided imagery induces a sense of empowerment and calmness, reduces anxiety and pain, boosts endorphin production, minimizes blood loss, and diminishes the need for pain medication among patients undergoing coronary artery bypass graft procedures. Other studies have shown a significant improvement of other postoperative pain management with the use of guided imagery.
To begin implementation, explain what will be happening and ask the patient to describe a place that brings them peace. Encourage your patients to find a quiet and comfortable space to relax. Then, instruct them to close their eyes (or look down) and take slow, deep breaths. Next, guide them to imagine their serene and soothing place, such as a beach, a forest, or a meadow. Use descriptions of the scene that include all five senses, asking them to imagine what they see (the blue sky), what they feel (the gentle wind on their face), what they smell (the richness of the forest smell) or hear (the birds calling and the leaves rustling). Add more detail. It helps to be there with them in your mind, imagining what you would see, hear, smell, taste, and feel. In this tranquil mental space, they can now visualize their pain as a physical object or sensation. Have them describe it… and then work on manipulating or diminishing it. This response might involve changing the color, shape, or size of the pain or simply letting it dissipate into the surroundings. Encourage them to use all their senses to immerse themselves in this experience. One example from a patient with RSD chronic pain visualized her pain as a pokey grey monster, but she found she could visualize petting it and calming it, so it was less frightening when she was done.
Researchers have studied image guidance in various types of settings, including postoperative, PACU, ICU, emergency room settings, and, most recently, pain management in COVID-19 patients. One study suggested guided imagery as an affordable, user-friendly, and straightforward complementary medical approach for addressing anxiety and pain in COVID-19 patients; thus, guided imagery may enhance relaxation and strengthen patients' immune responses in their battle against COVID-19 (Parizad et al., 2021).
Hypnosis
The integration of hypnotherapy into clinical settings promises a new dimension in pain management. While hypnosis was endorsed by the American Medical Association in 1958, it has fallen out of practice because of the creation of pharmaceuticals. There is a paradigm shift, and more physicians are referring chronic pain to treatment with guided imagery and hypnosis. There is a growing body of evidence supporting the effectiveness of hypnotherapy as a complementary tool in our caregiving arsenal (Tinelli et al., 2022).
Hypnotherapy involves guiding patients into a state of focused attention and deep relaxation and is used to help ameliorate pain, reduce anxiety, and facilitate healing. Patients undergoing hypnotherapy have reported reduced pain perception, decreased anxiety, and a diminished need for pain medications. Hypnotherapy has demonstrated effectiveness in various conditions, including chronic pain, surgery, childbirth, and palliative care. In a broader context, hypnosis has the potential to enhance the management of pain in emergency departments, pre or post-op, and other settings.
By inducing a state of deep relaxation and heightened focus, skilled hypnotherapists guide patients into a trance-like state where they can address and reframe their perception of pain. The process often begins with guided imagery, and then the patients are guided deeper into calm. This process often leads to reduced pain intensity, decreased reliance on pain medications, and enhanced coping mechanisms. Hypnotherapy can be particularly effective in managing chronic pain conditions, such as fibromyalgia or lower back pain, by assisting patients to manage discomfort and stress more effectively. Its non-invasive nature, lack of real side effects, and the potential to empower patients in their healing process make hypnotherapy a valuable tool in pain management. As a nurse, incorporating hypnotherapy into patient care plans can provide an additional avenue to enhance their overall quality of life and comfort during their medical journey.
Patients and healthcare professionals may have reservations about the mysterious nature of hypnosis, which can lead to skepticism or misunderstandings about its principles and practices. This can be addressed through education and by fostering a sense of trust. Hypnosis should not be used as a standalone treatment for severe or acute pain, and its integration into pain management should be in conjunction with traditional medical interventions. Clear communication, informed consent, and the normalization of using hypnotherapy help its use in various settings (Tinelli et al., 2022).
Massage
Massage is a body/skin manipulation technique that has been used around the world for eons. It was referenced in Babylonia (900 BC), China (2700 BC), India (1500-120 BC), Greece by Hippocrates (460-377 BC), Rome by Plato (427-347 BC) and Socrates (470-399 BC) and in the original Olympics (776 BC) for the athletes. There are many types of massage therapy techniques. For example, Swedish or Classic massage utilizes five different stroking movements, and deep tissue massage is a technique that does not seem to have a universally agreed-upon definition. With so many massage therapy techniques, it is not unexpected that studies report a wide range of results (25% to 100%) in pain reduction, with some types more consistently 60%-71% reported reduction in pain (Miake-Lye et al., 2019; Sahraei et al., 2022).
Substance P is found in the dorsal horn of the spinal cord, and elevated levels are known to be associated with chronic pain conditions. Massage therapy has been shown to reduce the level of Substance P in the saliva (Keeratitanont et al., 2015). An increase in muscle blood volume and skin blood flow has been reported at the site of the massage, as well as a reduction in pain intensity. There is speculation that the increase in blood flow could result in decreased Substance P levels and a reduction in the waste metabolites, such as lactic acid in the area, which results in decreased pain and a return to normal peripheral function. Other studies report an increase in oxytocin and the release of endorphins and serotonin with massage therapy.
Some of the most compelling research demonstrates how brain activity, as measured by an electroencephalogram, is affected by massage therapy. Dull pain sensation travels to the brain at a rate of 0.5 to 2 miles per second and sharp or burning pain sensation travels to the brain at 5-35 miles per second. According to the Gate Control Theory, since touch sensation travels to the brain at 35-75 miles per second, the brain will focus on the touch sensation instead of the pain sensation. Gate Control Theory is well documented and researched. Gate Control Theory is often used during childbirth for labor pain. If the patient fills all their senses with pleasant stimuli (lemon drop in mouth, gentle heat on skin, calming music, pictures of loved ones or favorite places, and pleasant aromas) then the numerous sensations coming in override the pain signals.
Other persuasive research shows that massage therapy affects the autonomic nervous system. Reduction in heart rate and blood pressure was shown during massage therapy sessions. This reflects that the parasympathetic nervous system is being triggered (Miake-Lye et al., 2019). The effect of massage therapy on muscle tension is also significant. Feelings of tightness, cramping, and spasms can be addressed with massage therapy, and thereby reducing pain.
Acupuncture
Acupuncture is a Traditional Chinese Medicine (TCM) treatment that is believed to have been in use for 2,500 years. It is a system of medical treatment that incorporates diet, exercise, herbs, spirituality practices, as well as acupuncture. It usually uses 5 to 20 small stainless steel, flexible needles, 10 to 100mm in size, placed into specific points on the body. Acupuncture is based on underlying philosophical principles of Confucianism and Taoism. These principles are the belief that individual health comes from the alignment of the qi, or “vital energy,” and acupuncture encompasses yin/yang, and uses these to realign the qi, the energy flow in the body. Acupuncture has been used for decades in the United Kingdom’s (UK) National Health Service and other evidence-based countries, but the public in the United States is generally not aware of the potential benefits.
Acupuncture in the treatment of chronic pain has not been fully embraced by the US, even though it is available at many of the top academic medical centers. While it is not known how acupuncture works, there is strong evidence of its effectiveness and is recommended by the World Health Organization for more than 100 conditions. Let’s be real, we still do not know how aspirin works. One theory of acupuncture is that needle stimulation influences inflammatory markers. Another is that needle stimulation induces hormonal changes. A third postulates the pressure itself influences loose connective tissue which causes immunomodulation. Another posits that analgesia results from the release of analgesics at the spinal and supraspinal levels, such as enkephalins and endorphins. And yet another, the Neurohumoral hypothesis, which is based on more than 100 scientific papers, theorizes that, in part, the pain-relieving properties are associated with the stimulation of nerve fibers in the horn of the spinal cord, which causes a cascade of endorphins (USDHHS, 2022; Vickers et al., 2023). While there are many theories, studies using functional MRIs have shown physiologic changes in the central nervous system in patients undergoing acupuncture. Traditional Chinese Medicine talks about how it clears the flow of energy through the body.
There have been many studies and systematic reviews of the efficacy of acupuncture in chronic pain. Because acupuncture is an individualized treatment that uses different points on the body, with different manipulation manners used by practitioners, different lengths of treatment, and different patient desired responses, it is impossible to develop a standardized treatment. There is some good research to support its use. The fact that The American College of Physicians recommends acupuncture as a first-line treatment for chronic low back pain and the National Institute of Healthcare Excellence suggests the use of acupuncture for chronic headaches and migraines demonstrates more acceptance for the use of acupuncture for chronic pain.
Nursing Implications
There might be skepticism or resistance to alternative or complementary therapies in the healthcare system, which can hinder the integration of these approaches into standard pain management protocols. Proper education, rapport, and implementation are the keys to providing patients the tools to overcome the complications of chronic pain. These techniques do take a nurse’s time away from other tasks and other patients, so it may not always be possible.
Implementing many of these techniques for pain management requires training and expertise to effectively guide patients through the process. Opportunities for nurses to be certified or at least further trained in these techniques are available. It does take some practice for nurses to become skilled at these techniques, but it empowers patients to take control of their pain and reduce their reliance on medication or other pain management techniques. We must also help assess and treat the whole patient. Depression and anxiety have an influence on the intensity of pain, so by addressing depression and anxiety, pain may also be reduced.
Other pain control methods a nurse might want to offer for the patient to explore with their doctor are physical therapy and exercise, topical medications, short term use of NSAIDS, corticosteroids, nerve blocks, epidurals, spinal cord stimulation, ultrasound, TENs, traction, or cognitive behavioral therapy referral. The type of pain, duration, intensity, and the patient’s perception of the meaning of the pain are all relevant to choosing which approaches may be best, and as always, the teaching is individualized, considering costs, access, and support. We hope to encourage more nurses to join us in this exploration of the other possibilities, training, and certification, where the power of the mind converges with the art and science of nursing to provide holistic and compassionate care.
Charlotte is an outpatient clinic charge nurse at Vanderbilt University Medical Center. She has been an RN for 11 years and ten years of that has been with Vanderbilt, and is a clinical hypnotherapist.
Amber Lauer is a Medical Aesthetics Mental Health Nurse Practitioner who focuses on the whole being in all aspects of primary care. Amber is a clinical hypnotherapist.
Dr. Wilson is the Chair of Excellence and Professor at Austin Peay State University School of Nursing and was the 2017 Holistic Nurse of the Year. Debra Rose uses hypnotherapy and other modalities to help patients manage pain.
Article references
- (2023). Understanding the Opioid Overdose Epidemic. https://www.cdc.gov/opioids/basics/epidemic.html
Keeratitanont, K., Jensen, M. P., Chatchawan, U., & Auvichayapat, P. (2015). The efficacy of traditional Thai massage for the treatment of chronic pain: A systematic review. Complementary Therapies in Clinical Practice, 21(1), 26-32. https://doi.org/10.1016/j.ctcp.2015.01.006
Miake-Lye, I. M., Mak, S., Lee, J., Luger, T. M., Taylor, S. L., Shanman, R., Beroes-Severin, J. M., & Shekelle, P. G. (2019). Massage for Pain: An Evidence Map. Journal of Alternative and Complementary Medicine, 25(5), 475–502. https://doi.org/10.1089/acm.2018.0282
National Institute on Drug Abuse [NIDA]. (2023). COVID-19 & Substance Use. https://nida.nih.gov/research-topics/comorbidity/covid-19-substance-use
Parizad, N., Goli, R., Faraji, N., Mam-Qaderi, M., Mirzaee, R., Gharebaghi, N., Baghaie, R., Feizipour, H., & Haghighi, M. M. (2021). Effect of guided imagery on anxiety, muscle pain, and vital signs in patients with COVID-19: A randomized controlled trial. Complementary therapies in clinical practice, 43, 101335. https://doi.org/10.1016/j.ctcp.2021.101335
Sahraei, F., Rahemi, Z., Sadat, Z., Zamani, B., Ajorpaz, N. M., Afshar, M., & Mianehsaz, E. (2022). The effect of Swedish massage on pain in rheumatoid arthritis patients: A randomized controlled trial. Complementary Therapies in Clinical Practice, 46, 101524. https://doi.org/10.1016/j.ctcp.2021.101524
Tinelli, M., Guler, N., Goetz, C., Aim, P., Marchionni, S., Ouamara, N., Cipolat, L., Demarquet, M., Seris, E., Moreau, A., Durand, G., Douplat, M., Lavignon, J.-P., Hingray, C., & Abensur Vuillaume, L. (2022). Study protocol: Hypnosis versus standard care for shoulder dislocation reduction in the emergency department - a multicentre, randomised, controlled study protocol. British Medical Journal Open, 12(12), e062278. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9730355/
U.S. Department of Health and Human Services [USDHHS], (2022). Acupuncture: What you need to know. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/acupuncture-what-you-need-to-know
Vickers, A. J., Cronin, A. M., Maschino, A. C., Lewith, G., MacPherson, H., Foster, N. E., Sherman, K. J., Witt, C. M., Linde, K., & Acupuncture Trialists’ Collaboration, for the. (2012). Acupuncture for chronic pain. Archives of Internal Medicine, 172(19), 1444. https://doi.org/10.1001/archinternmed.2012.3654
Click an image to expand viewer.

Debra Rose Wilson, PhD MSN RN IBCLC AHN-BC CHT

Charlotte Chavous, BSN, RN, AMB-BC, CHT

Amber Lauer, MSN, APRN, FNP-BC, CHT
-
Above Photos Left to Right - Debra Rose Wilson, PhD MSN RN IBCLC AHN-BC CHT > Charlotte Chavous, BSN, RN, AMB-BC, CHT > Amber Lauer, MSN, APRN, FNP-BC, CHT
Spotlight on Nursing Fundamentals
Preventing Falls in the Hospital Setting: A Nursing Guide
 Cassand Dodson, RN-BSN, MSN
Cassand Dodson, RN-BSN, MSN
Falls are a significant concern in the hospital setting, posing serious risks for patient safety and well-being. As nurses, we play a crucial role in preventing these potentially devastating events. This article explores evidence-based strategies and interventions to minimize fall risk, drawing on the latest research and best practices.
Understanding the Scope of the Problem
Falls are alarmingly common in hospitals, affecting an estimated 30% to 50% of patients. These incidents can lead to various injuries, ranging from minor bruises and fractures to severe trauma and even death. Moreover, falls can significantly impact patient morale, prolong hospital stays, and increase healthcare costs.
Identifying Fall Risk Factors
Early identification of patients at high risk of falling is crucial for implementing preventive measures. Numerous factors contribute to fall risk, categorized into intrinsic (patient-related) and extrinsic (environmental) factors:
Intrinsic factors:
- Age (over 65 years)
- Cognitive impairment
- Gait and balance problems
- History of falls
- Weakness and decreased muscle strength
- Visual impairments
- Medications (e.g., sedatives, diuretics)
- Dehydration
- Pain
Extrinsic factors:
- Wet or slippery floors
- Poor lighting
- Cluttered environment
- Unstable furniture
- Inadequate bed brakes and side rails
- Lack of assistive devices (canes, walkers)
- Footwear with poor traction
- Implementing a Multifaceted Approach
Preventing falls requires a comprehensive approach incorporating various interventions on both individual and environmental levels. Here are key strategies:
Universal Fall Precautions:
These precautions apply to all patients, regardless of their perceived fall risk. They create a safe environment and promote patient awareness:
- Maintaining a safe environment: Keep floors clean and dry, ensure adequate lighting, eliminate clutter, and use non-skid mats.
- Bed positioning: Keep bed in the lowest position when unoccupied and at a comfortable height for transfers. Lock bed brakes and side rails appropriately.
- Call light accessibility: Ensure the call light is within reach and patients understand its use.
- Footwear: Encourage patients to wear well-fitting, closed-toe shoes with good traction.
- Patient education: Inform patients about fall risks and encourage them to call for assistance before attempting ambulation.
Individualized Fall Risk Assessment:
Use validated fall risk assessment tools like the Morse Fall Scale or the Hendrich II Fall Risk Model to identify high-risk patients.
Regularly reassess fall risk as factors can change during hospitalization.
Individualized Interventions:
- Strengthen mobility: Encourage early mobilization as tolerated and provide physical therapy if needed.
- Address medication concerns: Work with physicians to review medications with fall risk potential and consider safer alternatives.
- Visual and hearing aids: Ensure patients have access to corrected vision and hearing aids, if necessary.
- Manage pain effectively: Uncontrolled pain can affect balance and gait, so proper pain management is crucial.
- Cognitive impairment interventions: Supervise patients with cognitive impairment closely and implement environmental modifications like cognitive aids.
- Assistive devices: Provide and train patients on using appropriate assistive devices such as canes, walkers, or grab bars.
Communication and Collaboration:
- Effectively communicate fall risk assessments and individual interventions to the entire healthcare team.
- Encourage family involvement in fall prevention efforts.
- Conduct debriefings after fall incidents to analyze contributing factors and implement corrective measures.
Evidence-Based Interventions:
Multicomponent fall prevention programs: Studies have shown that multifaceted programs combining various interventions, such as patient education, environmental modifications, and exercise, can significantly reduce fall rates.
Alert systems: Using wearable devices or bed sensors, patient monitoring systems can alert staff of potential falls. However, their effectiveness needs further investigation and careful consideration of potential downsides like alarm fatigue.
Strength and balance training: Targeted exercise programs can improve patient strength, balance, and gait, reducing fall risk.
Conclusion
Preventing falls is a shared responsibility within the healthcare team. By implementing the strategies outlined above, nurses can play a crucial role in keeping patients safe and preventing the devastating consequences of falls in the hospital setting. Remember, early identification, comprehensive assessment, and evidence-based interventions are key to success. Let's work together to create a culture of safety and minimize the risk of falls for our patients.
Article references
Agency for Healthcare Research and Quality. (2020). Preventing Falls in Hospitals. Retrieved from: https://www.ahrq.gov/patient-safety/settings/hospital/fall-prevention/toolkit/index.html
Centers for Disease Control and Prevention. (2023). Falls Among Older Adults. Retrieved from: https://www.cdc.gov/falls/index.html
Nurses Well-Being
How To Heal from Burnout and Love Nursing Again
 Shenell Thompkins, RN, MSN
Shenell Thompkins, RN, MSN

In addition to caring for patients, nurses often take care of everyone else while neglecting themselves. So, who takes care of the nurse while the nurse takes care of everyone else?
Key topics: the nursing profession, burnout, self-care, and resilience.
The Nursing Profession and Where We Stand
The 2023 State of Nursing Report prepared by Nurse.org revealed the realities of nursing, and there are a few things worth highlighting.
- When asked why they became a nurse, the primary response from nurses was “to help others.” The second most common response was due to the specialties and career options of choice.
- Of those polled, 60% of nurses said they "love being a nurse," but 62% of nurses are concerned about the future of nursing.
- A whopping 81% of nurses said they have felt burnt out in the past year, slightly less than in 2021.
It's heartwarming to know that nurses still have an innate love for their profession and the desire to help others.However, 81% is a significant number of nurses who responded that they felt “burnt out.” Despite nursing being an admirable profession, this burnout is projected to contribute to the ongoing nursing shortage.
According to the American Association of Colleges of Nursing (AACN), the Registered Nurse (RN) workforce is projected to increase by 3.3 million nurses by 2030. However, 203,000 RN openings are expected annually leading up to 2030.
These findings are based on retired nurses and those who are potentially going to leave the workforce. The nursing shortage is further exacerbated by an aging population, which will result in a higher demand for medical care. Additionally, there are restricted nursing school enrollments due to a shortage of nursing school faculty and understaffing in the healthcare setting in general (AACN, 2022). This seems to be creating a never-ending cycle of problems.
Burnout: Self-Assessment and Awareness
With that being said, the following questions should be asked of all nurses:
- Do you feel emotionally drained?
- Do you wake up feeling exhausted after an adequate amount of sleep?
- Do you dread going to work?
- Do you find yourself insensitive to the things you would usually be empathic toward?
- Do you think about quitting your job often?
- Do you find yourself more cynical or judgmental?
- Do you no longer find joy in going to work?
If most of these questions are answered with a yes, one may be experiencing signs and symptoms of burnout. Experiencing burnout throughout a nurse's career may be inevitable, and it's important to know what it is and how to prevent it when possible.
Burnout is a state of emotional exhaustion, depersonalization, and feeling drained, as defined in the Future of Nursing, 2020-2030 report. This condition can cause nurses to lose interest in their jobs and become less empathetic toward their patients.
Burnout can lead to high turnover rates, negative patient outcomes, personal illnesses, and even suicide. While there is no definitive solution to overcoming burnout, nurses can start by taking control of their priorities and caring for themselves. This requires being intentional and bringing the best version of themselves to the work environment. Another name for this is self-care.
Self-Care – Making the Necessary Changes
Iyanla Vanzant says it best, "My cup runneth over; what comes out of the cup is for y'all, but what is in the cup is mine, so I have to keep my cup full."
In other words, you cannot pour from an empty cup, so metaphorically, do not attempt to pour from an empty cup in your own life. You have to take care of yourself and keep your cup full.
According to the National Institute of Mental Health, self-care is taking the time to do things necessary for an individual's overall well-being. Well-being includes physical and mental health, whereas one or both can be unhealthy. It is essential to strive to be the best version of yourself while also wanting the best for your patients and peers.
Keith Carlson emphasizes that self-care is not rocket science and can differ from person to person in his Nurse.org article "5 Simple Self-Care Practices For Busy Nurses. We're Not Talking A Spa Day | Nurse.org,"
Keith explains how to use the nursing process to identify your self-care needs. He suggests performing a self-assessment, diagnosing any self-care deficits, planning a course of action, implementing the plan, and evaluating your progress.
Here are some helpful tools and knowledge to promote physical and mental health, whether to address self-care deficits, improve upon them, or simply be more intentional about caring for oneself.
Let’s break self-care down even more.
Physical Health
- Regular exercise
- 150 minutes per week of moderate-intense aerobic activity or 75 minutes of vigorous aerobic activity is recommended by the American Heart Association. *Start small and remember consistency is key.
- Fitness Apps
- YouTube videos
- Active Gym Membership(s)
- Live workouts on social media
- Yoga or Pilates
- Healthy Diet
- Eating a well-balanced diet of fruits, vegetables, and protein
- Limit sugar and sodium intake
- Limit pre-packaged foods
- Reduce consumption of fried foods and fat intake
Check out High protein & high energy snacks for nurses on Nurse.org for more ideas.
- Stay Hydrated
- 13 cups of daily fluid intake are recommended for men, and 9 cups of daily fluid intake is recommended for women, according to the Institute of Medicine (IOM).
- Limit caffeine, sodas, and alcohol
Mental Health
In addition to exercise, diet, and improving your physical health, here are some other ways to improve your mental health.
- Rest
- Make rest a priority by creating a sleep routine and taking a vacation or days off work as scheduled.
- Stay Positive
- Focus on positivity by finding things you are grateful for and challenging your unhelpful thoughts.
- Support
- Create a support system by finding ways to destress and have an outlet.
- Spiritually - return to what gives you meaning and get grounded in your faith, hope, and beliefs.
- Socially - be intentional in occasionally meeting with family, friends, or associates and socializing.
- Habits, interests, or hobbies - get creative and start doing things you used to love to do when you were younger: color, draw, write, build things, read books, or explore something new!
- Professionally - seek professional help and counseling services if you find yourself feeling depressed, stressed, suicidal, anxious, or need guidance.
- Set Boundaries
- It's okay to say “no” and be okay when others say “no”
- Boundaries protect your overall well-being and others
- These boundaries may include physical, sexual, mental, emotional, financial, and/or time boundaries
- Check out How To Set Boundaries at Work as a Nurse by Nurse Alice for more details on how to set boundaries and why it's important
Check out 7 Tips To Help Nurses Be Physically, Mentally, and Emotionally Healthy
Resilience - Keep moving forward
Resilience is the ability to overcome challenges while remaining optimistic for the future. Resilience may also help nurses cope with feelings of burnout (JONA, 2020).
Focusing on self-care can help nursing professionals become more self-aware and develop coping mechanisms to navigate the challenges of their profession. Most nurses choose this career path because they strongly desire to help others, demonstrating strength, compassion, empathy, and selflessness. However, nurses must also practice what they preach and prioritize their own self-care, just like they would for their patients, family, friends, and community. This is important to avoid burnout and ensure they remain healthy and effective in their caregiver roles.
Board of Nursing Update
Board of Nursing Update - September 2024
 Sherry Richardson, MSN, RN - Executive Director
Sherry Richardson, MSN, RN - Executive Director

1.) Licensing/Regulation
- Board member vacancy: Public Member.
- Government Operations Committee approved updated Comprehensive RN, LPN, APRN comprehensive rules packet September 18, 2024.
- Updated rules will go into effect October 2024. These rules will be available at the following link: https://publications.tnsosfiles.com/rules/1000/1000.htm
2025 Board of Nursing Meeting Dates:
- February 19-20
- May 14-15
- August 6-7
- November 19-20
2.) Nurse Licensure Compact (NLC)
- 42 jurisdictions have joined, 39 have implemented.
- On January 2, 2024, a new NLC rule went into effect. Nurses relocating to another compact state have 60 days from the time they move to apply for a new license by endorsement in a new primary state of residence. Information may be found at NLC.gov.
TSU Receives Continuing Accreditation Through Fall 2031

The Tennessee State University School of Nursing is proud to announce that the Bachelor of Science in Nursing (BSN) program underwent a continuing accreditation site visit during the Fall 2023 semester and has received continuing accreditation from the Accreditation Commission for Education in Nursing (ACEN) through Fall 2031. The BSN program also has full approval by the Tennessee Board of Nursing (TBON). For more information about the BSN program please visit our website: TSU BSN Program
Government Affairs
TNA Lobbyist Report
 Garrett Johnson, Director of Government Affairs & Chief Lobbyist
Garrett Johnson, Director of Government Affairs & Chief Lobbyist

In West Tennessee, Sarah Freeman won a five-way Democratic primary in Congressional District 8 and will now try to unseat Congressman David Kustoff in November. Moreover, Democratic incumbent Steve Cohen had a strong primary showing and won a four-way race with over 73 percent of the vote. He will now face Charlotte Bergmann in the general election.
State Senate Election Results
This election cycle, 16 of Tennessee’s 33 Senate seats are on the ballot, with nine of those 16 seats having contested primaries.
Tom Hatcher won a three-way GOP primary in Senate District 2, which is currently an open seat with the retirement of Sen. Art Swann.
As was mentioned earlier, two incumbent Senators lost their primary elections, which was the first time since 2016 that a Republican state Senator lost such race. Jon Lundberg, who has been a champion for nurses in the past, lost his race by less than 1,000 votes, while Frank Niceley was defeated in the state’s 8th Senatorial District.
The biggest primary election victory for nurses was Sen. Ferrell Haile (R-Gallatin) winning his hotly contested race in District 18. Senator Haile has been a friend to the nursing profession throughout his tenure, and we are pleased that he was victorious. The remaining Senate districts saw incumbent Senators Becky Massey (R-Knoxville), Todd Gardenhire (R-Chattanooga), Ken Yager (R-Kingston), John Stevens (R-Huntingdon), and Sara Kyle (D-Memphis) all win primary races.
State House Election Results
The state House saw 29 of its 99 legislative seats have contested primary elections. The biggest upset of the entire day was Rep. Hazlewood, chairwoman of the powerful House Finance Committee, losing her District 27 race to Michele Reneau, while her colleague and fellow chairman, John Ragan, lost to Rick Scarbrough in the 33rd House District. The remaining House primaries went largely as planned with incumbent Representatives Robert Stevens (R-Smyrna), Sam McKenzie (D-Knoxville), Kevin Raper (R-Cleveland), Yusuf Hakeem (D-Chattanooga), Ron Travis (R-Dayton), Tim Rudd (R-Murfreesboro), Paul Sherrell (R-Sparta), Bob Freeman (D-Nashville), Scott Cepicky (R-Culleoka), Chris Todd (R-Jackson), Rusty Grills (R-Newbern), Mary Littleton (R-Dickson), Johnny Shaw (D-Bolivar), Joe Towns (D-Memphis), Justin Pearson (D-Memphis), G.A. Hardaway (D-Memphis), and John Gillespie (R-Memphis) all winning.
Looking Ahead
All eyes now turn to the general elections on November 5th, and as was the case in the primaries, voter turnout could play a key role in the upcoming general. The presidential election at the top of the ticket will certainly drive individuals to the polls, which should result in more votes cast for down ballot candidates. A race that is sure to capture the attention of many will be held in the 7th Congressional District in middle Tennessee, where incumbent Congressman Mark Green is being challenged by former Nashville Mayor Megan Berry. At the state level, only a handful of races are likely worth watching, most notably in Shelby and Davidson counties. While many of the 132 legislators have November races, most of the significant battles took place during the primaries.
TN Nurses PAC
Your TN Nurses PAC
 Marcia Barnes, DNP, ACNP-BC, CWS, CPSN, TNA Chair-TN Nurses PAC
Marcia Barnes, DNP, ACNP-BC, CWS, CPSN, TNA Chair-TN Nurses PAC

Nurses are natural leaders, and government needs more nurses to get involved and provide leadership benefits in healthcare to our communities and our profession. One of the responsibilities of nursing is to take an active role in politics and policy development, but so few do. Why do nurses not participate in lobbying efforts? There are likely many reasons. Some reasons include poor nursing images, feelings of inefficacy in influencing political decision-making, perspectives of public policy advocacy as not in the scope of the nurse's professional role, lack of confidence and mentorship, and insufficient knowledge of policy-making strategies. One of these may be the reason you, like most nurses in Tennessee, aren’t involved actively in policy. We all experience issues that impact how we provide care to patients daily. The shortage of nurses and healthcare policy changes are two politically important issues that will affect all nurses in Tennessee. The impact on patient care can be widespread, including longer wait times, decreased access to care, provider shortages, and increasing workload for nurses. These are issues that hit home, and it is why all Tennessee nurses need to be active in policy development and advocacy. All nurses want to provide the best possible care.
The TN Nurses PAC is bipartisan and supports members of the Tennessee Legislature who have demonstrated a commitment to the initiatives of the GOVA Committee and Tennessee Nurses Association and/ or hold valuable positions on key committees. Recently added to the PAC website is a list of recipients of PAC donations for 2023. The PAC Board has already approved donations for 2024 and will continue to identify, with the help of TNA’s lobbyist, where additional funds may be needed. So why make these contributions? These contributions provide visibility for nurses in Tennessee and ensure we have a seat at the table with legislators working on healthcare issues. For nurses, a seat at the table is better than just being on the menu. It also helps build strong relationships with legislators that may be an asset in our future endeavors. Through advocacy and monetary support, your TN Nurses PAC assists campaigns, policy proposals, legislative initiatives, and the candidates that support the nursing profession. We know that our nursing priority is bringing the best possible care to our patients and the residents of Tennessee. The priority of the PAC is to help accomplish this goal.
Members of the Tennessee Legislature frequently hold fundraising events in their districts. This is especially the case with elections. These events serve as a venue for political networking and personal connections. Many of these events carry steep entry fees of $1000 or more. The TNA lobbyist attends many of these events with the support of our PAC. This is where nurses come in! TN Nurses PAC pays the cost for our lobbyist to attend these events, providing an opportunity to make personal connections and foster relationships with legislators and their staff. Events like this often hold the key to gaining long-term support from members of the Legislature. The PAC provides an organized way for nurses to support political candidates, causes, legislation, regulations, or initiatives supporting healthcare issues important to Tennessee nurses and residents. Donating to our PAC is a simple way for nurses who share common goals and interests to have their voices heard within our political system and become active advocates.
The 113th General Assembly has adjourned. We can only look forward to the 114th General Assembly in 2025. The Tennessee Nurses Association must continue to be avid in developing our relationships, and the PAC must continue making donations. This being an election year, TNA will likely see new faces in the Legislature as well as on those key committees. This will necessitate ongoing relationship building. I am happy to report that the TN Nurses PAC has been able to donate to candidates in 2024 who are TNA and nurse-friendly. This is made possible only with your continued donations, so consider making a donation today!

American Nurses Association (ANA) Membership Assembly Update
 Ray Coe, PhD, MBA, MHA, RN-BC, NEA-BC, FACHE(R)
Ray Coe, PhD, MBA, MHA, RN-BC, NEA-BC, FACHE(R)

ANA Hill Day occurred on 27 June 2024. It was record-setting, with 481 RNs and nursing students meeting with members of Congress or their staff in our nation’s capital in support of the following bills and regulations:
- Restricting Mandatory Overtime for Nurses (H.R. 7546, S. 3860)
- Nurse Faculty Shortage Reduction Act (H.R. 7002, S. 2815)
- Improving Care and Access to Nurses (ICAN) Act (S. 2418, H.R. 2713)
- Protect Timely Access to Quality Nursing Care in LTC Facilities.
This advocacy day took place before the annual ANA Membership Assembly (MA) meeting, June 28-29, 2024, when delegates from ANA’s constituent and state nurses associations (C/SNAs), the Individual Membership Division, and organizational affiliates gathered to discuss and determine the association’s positions on key issues for nurses and the nursing profession.
ANA Interim CEO Angela Beddoe described the need for ANA to advance its current operational and strategic priorities and consider how “our decisions affect us not only one year from now but fifteen years from now.” With the future in mind, she described an Integrating Excellence Initiative ANA is undertaking to meet nursing’s needs between now and 2040. More information on the Integrating Excellence Initiative will be shared in the Fall. (See “A Message from ANA CEO, Angela Beddoe” in this issue)
The MA voted to support seeking licensure and employment reform to combat mental health stigma. It is often associated with substance abuse, but it was reported that all forms of mental health issues may be held against a nurse seeking employment or license renewal. If we do not hold it against someone for seeking physical health treatment, why mental health treatment? The MA voted to strive to improve care for the veteran population by seeking to improve training regarding the unique health care needs of the veteran population, including TBI, resp distress due to burn pit smoke, etc. The 2025 Code of Ethics revisions were reviewed, and changes were proposed. The revisions are awaiting final review.
Additionally, ANA’s Automatic Dues Escalator passed beginning in January 2025. For individuals who have been paying $15.00 per month, the rate will go up to $15.75 per month. For annual payors who have been paying $174.00 per year, the new rate will be $183.00 per year. While the increase is effective January 1, 2025, the increase will not go into effect until the anniversary date of your membership after January 1, 2025. Premier members will be notified of the new rates as soon as they are released by ANA. After an extended debate, ANA voted not to endorse a presidential candidate. Finally, ANA voted to review and expand our business ethics practices by agreeing that those with whom we do business should follow the same ethics standards as ANA.
ANA elected the following officers and positions;
- President Jennifer Mensik Kennedy, PhD, MBA, RN, NEA-BC, FAAN,
Oregon Nurses Association; - Secretary Amanda Oliver, BSN, RN, CCRN, CPST, ANA-Illinois;
- Director-at-Large Edward Briggs, DNP, MS, APRN, Florida Nurses
Association; - Director-at-Large Ahnyel Burkes, DNP, RN-BC, NEA-BC, Louisiana State
Nurses Association; and - Director-at-Large, Staff Nurse Josephine Agyei, BSN, RN, ANA-New York.
Elected to serve on the Nominations and Elections Committee are:
- Mavis Mesi, DNP, MSN, RN, Colorado Nurses Association;
- Vinciya Pandian, PhD, MBA, MSN, RN, ACNP-BC, FCCM, FAANP,
FAAN, FFNMRCSI, Maryland Nurses Association; and - Kimberly Velez, MSN, RN, ANA-New York.
A Message from ANA CEO, Angela Beddoe
 Angela Beddoe, ANA CEO
Angela Beddoe, ANA CEO

It is my honor to accept the position of ANA Enterprise CEO, and I am thankful to the ANA board of directors for their faith in me. Over 100 days ago, I came to this organization and met some of the most passionate and dedicated employees at ANA along with esteemed leaders who guide ANA, ANCC, and the Foundation boards as well as leaders who have been at the helm of ANA in the past and continue to provide tremendous wisdom.
You all inspire me. I am also inspired every day by the brilliant leaders of our Constituent and State Nursing Associations and organizational affiliates and have been ever so humbled by their commitment and dedication. I am deeply moved to be able to work with so many who dedicate their lives to helping others.
In June, at Membership Assembly, I shared a little bit more about myself, my thoughts, and vision for ANA. If you were unable to attend, you can watch the recording of my speech below.
I am excited about ANA Enterprise and all its possibilities. I am excited about the work we will be doing, Imagining ANA into 2040 and I look forward to working with you all as we co-create a strategy and to shape the future of nursing and health care.
With dedication and deepest appreciation,
Angela
Angela Beddoe
ANA Enterprise Chief Executive Officer

A Lesson in Compassion
 Kelly Carrel, RN
Kelly Carrel, RN

There are many aspects to being a nurse, such as knowledge, competence, experience, critical thinking, good judgment, and compassion. Throughout the course of performing a long list of tasks, it can be very easy to forget that the people we are taking care of are more than just a list of duties. It can also be easy to forget that while we are watching the patient throughout the day, they too, are watching us. I have been in both positions: the patient and the health care provider. I am grateful that I was able to experience being a patient before starting to work at a hospital because it allowed me to have the true patient perspective without prior knowledge or bias.
It was May in 1998, and I had been working as a nurse technician for less than two years, all of which had been limited to the general nursing home setting. I had been working a lot of hours, and my home life was very stressful, so when I began to feel fatigued and weak, I overlooked it as symptoms of my environment. Even when I began having abdominal pain, I attributed it to ovulation. I continued my normal routine for two more weeks, never missing a day of work. Eventually, once I began vomiting uncontrollably, I conceded to go to my local hospital. I arrived at the ER breathless, pale, dizzy, and confused. I was immediately rushed into a room, accompanied by my husband and young daughter.
The nursing staff expressed irritation that I could not control my vomiting long enough to drink what seemed like copious amounts of a sickly sweet concoction of orange juice and CT contrast. I was embarrassed to be vomiting and felt ashamed by their irritation and obvious displeasure. I was told that I needed to cooperate with the nursing staff by drinking and holding down the oral contrast if I wanted them to help me. In the hall, I could hear the nurse telling someone about how I was “gasping for air all dramatically,” would not stay lying down like I was told, and would not stop “puking” long enough to drink the contrast. I felt humiliated by my weaknesses and kept apologizing profusely. I was taken to medical imaging for an abdominal CT. IV contrast was administered, and my vitals were taken, without a single word of kindness or compassion. I was the part of their job that they disliked, and I knew it. The vitals showed that my blood pressure had dropped to 32/20 and the CT showed that my abdominal cavity had completely filled with blood. Some of what happened afterward were lost in the shock and confusion, but some things stood out.
I heard the physician tell my husband I might not make it while my young daughter watched and listened in terror. Suddenly, things had changed. I had somehow morphed from the bothersome patient that the poor nurse got stuck with into a critical project. People seemed to come from nowhere and everywhere, all at once. Staff began barking medical terms at each other, talking about me, yet, I had no idea what was happening. Where were they taking me? Why would they not answer my questions? Where was my daughter and was she ok? Why would no one look in my eyes? I felt like an inanimate object in the room.
During the exploratory surgery, it was discovered that a blood vessel on my ovary had ruptured and I had been bleeding internally for approximately two weeks. I stayed in the hospital for a few days without any complications. During my stay, nursing staff would come in and talk to each other about the rotten management, their significant others, and their co-workers. I heard staff in the halls talking about certain patients and all the things the nurses wished they could say to them. I heard the nurse talk nicely to the patient across the hall from me, then shut the door and start making fun of them with another nurse as they walked down the hall. I wondered if she talked about me and the rest of the patients in the same manner.
I watched, I listened, and I learned. I learned the value of a gentle touch and genuine kindness. I learned the damage that a few thoughtless words could do, not only to the victim but to everyone hearing them. I learned that our patients are not just room numbers and not just assignments, but instead, they are living, breathing individuals with emotions and feelings. When a patient is hurting, feels alone, afraid, and drowning in a sea of uncertainty amidst all the chaos, I want them to know that I see them as an individual and I care.
I have now been in the medical field for 28 years, close to 10 of them as a Registered Nurse. I have never forgotten how it feels to be the patient: the fear, the vulnerability, the powerlessness, and unfortunately, sometimes the shame. I remember it every time I look into my patient’s eyes and see their fear and uncertainty. I remember it every time I speak with the families as they gather around me searching my face for some sign of hope. I remember it when I hold the weeping family that just lost their loved one and let my tears fall with theirs.
It’s far too easy to get caught up in the innumerable tasks in our job, but I pray we always remember the people we are trying to help … with compassion.
Microaggressions in Health Care – Part 1
 Georgita T Washington, , PhD, RN, MSN, MACM
Georgita T Washington, , PhD, RN, MSN, MACM

Dr. Chester Pierce first coined the term “microaggression” in 1970. The psychiatrist originally intended the term to refer to the more subtle form of racism that had existed during Jim Crow (Turner, Higgins, & Childs, 2021; Williams, 2021). They are the subtle snubs, slights, and outright insults directed to ethnic/racial minority groups, women, members of the LTBGQIA+ community, religious minorities, those with mental illnesses, and other marginalized people groups who are not seen to fit into the dominant societal norms. These less obvious but powerful negative forms of discrimination impact all marginalized people groups and include verbal and non-verbal interactions (Johnson, Nadal, Gina Sissoko, & King, 2021; Williams, 2021; Carter & McMillian-Bohler, 2021). Microaggressions occur within and among nursing and other healthcare professions. It also occurs between patients and health care professionals and vice versa (Burks & Olson, 2023; Pusey-Reid, Gona, Lussier-Duynstee, & Gall, 2022; Turner, Higgins, & Childs, 2021).
Several types of microaggressions have been identified in the literature (Carter & McMillian-Bohler, 2021Johnson, Nadal, Gina Sissoko, & King, 2021). Microassaults are verbal or non-verbal attacks intended to hurt the targeted individual. Microinsults are intended to humiliate or demean the targeted individual. Microinvalidations are meant to exclude or dismiss the thoughts, feelings, and lived experiences of those individuals. A fourth type has been reported as environmental microaggressions that occur in the context of the workplace or a specific environment (Carter & McMillian-Bohler, 2021; Johnson, Nadal, Gina Sissoko, & King, 2021). This can be thought of as an unhealthy work environment.
These behaviors are called “micro” because the actions are counted as trivial or harmless by those who are not part of the targeted group. However, the resulting trauma caused to the recipient is very real. Microaggressions in any form may be conscious or unconscious, may occur as the result of implicit bias, and are different from deliberate acts such as racial slurs, physical assaults, and overt racism (Ackerman-Barger, Boatright, Gonzalez-Colaso, Orozco, & Latimore, 2020). Microaggressions are considered by some to be a form of behavior and hostility that is thought to be socially unacceptable (Turner, Higgins, & Childs, 2021).
Microaggressions are problematic. They have been reported to cause physical, emotional, behavioral, and mental health problems for recipients of such behavior. Having to constantly experience, respond to, and explain these types of behaviors leads to increased stress and a chronicity of the stress response. This leads to poor physical health outcomes such as obesity, diabetes, and cardiovascular disease (Ackerman-Barger & Jacobs, 2020; Johnson, Nadal, Gina Sissoko, & King, 2021). Nurses and other health professionals, as well as their students belonging to minority and marginalized groups, have all reported bouts of depression, decreased mental function, and decreased professional productivity and academic performance. When the offender is a faculty member or in other supervisory positions, this places extra stress on the recipient because now they must consider retaliation and placing their position in the program in jeopardy, or the potential of a poor performance evaluation if they confront the offender (Ackerman-Barger, Boatright, Gonzalez-Colaso, Orozco, & Latimore, 2020; Carter & McMillian-Bohler, 2021).
Increased diversity and cultural competency in nursing and other health professions are necessary to help decrease health disparities and inequities in ethnic and communities of color (Carter & McMillian-Bohler, 2021). Research has demonstrated there are more positive outcomes in these people groups when the providers look like them. Microaggressions and blatant discriminatory behaviors have decreased the numbers of individuals choosing health care as a profession, as well as caused some to leave their chosen profession (Burks & Olson, 2023; Pusey-Reid, Gona, Lussier-Duynstee, & Gall, 2022).
When microaggressions go unchallenged, the offenders continue to “not know what they do not know” or continue to disrespect and devalue other human beings. When these behaviors are allowed to continue, they become structural or institutionalized because they are never corrected or called out as unacceptable. They become embedded in the culture, and when it is pointed out that these behaviors are hurtful to others, those complaining are seen as too sensitive or making excuses for perceived poor performance. These accusations themselves then cause more trauma and harm to the recipient, increasing the stress.
Consider these lived experiences of microaggressions as examples of behaviors to avoid and to bring attention to when coming from others.
- As a Black surgical resident reports to the operating room to begin her first case, the White charge nurse asks her if she is “the help,” voicing a preconceived assumption (Turner, Higgins, & Childs, 2021).
- A White patient asks a Black nurse if the nurse is the one “who is going to wait on me?” (Georgita Washington, personal experience)
- A White nurse notices the Black nurse has added braids since they last worked together. The White nurse reached to touch the braids, and the Black nurse backs up and says, “Please do not do that.” The White nurse responds with “y’all are so sensitive.” (Georgita Washington, personal observation)
- After being made aware of an inappropriate statement, the White Associate Dean tells a Black faculty member that she does not see the faculty as Black, which can be perceived as not seeing the faculty for who she is in her entirety (Georgita Washington, personal experience).
- A Black patient is exhibiting signs and symptoms of what would later be diagnosed as a stroke. The first question the White Emergency Department physician asks is, “Have you ever been incarcerated?” (Georgita Washington, personal observation)
- Statements that there would be more professionals of color if “they would quit whining and work harder” diminish and deny their lived experiences of overcoming barriers (Georgita Washington, personal observations).
- Statements such as “You people always make everything about race!” when challenged about inequities in health disparities deny the lived experiences of the recipients (Georgita Washington, personal observation).
- “You are so well-spoken for a Black person,” assumes that is an unusual and unexpected occurrence and that the statement is a compliment. The offender becomes irate when the recipient asks why they are surprised (Georgita Washington, personal experience).
- The experienced nurse who keeps interrupting the new nurse as they give a report, never really giving the new nurse an opportunity to finish a thought. The new nurse lost confidence in their ability to give a comprehensive report (Georgita Washington, personal observation).
Microaggressions have been defined and supported with examples of lived experiences. What is needed to eliminate these behaviors are intentional strategies. The strategies must be focused on decreasing the occurrence of microaggressions and their negative impact on both individual health, and the diversity of health care professionals. Strategies may include self-evaluation about the use and recognition of microaggressions, self-education about their meanings to and responses from recipients, and then being intentional about interactions with people from other groups that are different. Being willing to confront and correct, as well as willing to be confronted and corrected, will make for healthier individuals and environments (Ackerman-Barger & Jacobs, 2020; Ackerman-Barger, Boatright, Gonzalez-Colaso, Orozco, & Latimore, 2020; Carter & McMillian-Bohler, 2021; Burks & Olson, 2023; Pusey-Reid, Gona, Lussier-Duynstee, & Gall, 2022).
Specific interventions will be covered in a future article.
Article references
- Ackerman-Barger, K. & Jacobs, N.N. (2020). The Microaggressions Triangle Model: A Humanistic Approach to Navigating Microaggressions in Health Professions Academic Medicine. 95(12): S28-S32. doi: 10.1097/ACM.0000000000003692.
- Ackerman-Barger, K., Boatright, D., Gonzalez-Colaso, R., Orozco, R., & Latimore, D. (2020). Seeking Inclusion Excellence: Understanding Racial Microaggressions as Experienced by Underrepresented Medical and Nursing Students. Academic 95(5): 758 – 763. doi: 10.1097/ACM000000000003077.
- Burks, K. A. & Olson, L. (2023). Let’s Talk About It: Addressing Microaggressions in Occupational Therapy Education. American Journal of Occupational Therapy, 77(3), 1 – 4. org/10.5014/ajot.2023.050125
- Carter, B.M., McMillian-Bohler, J. (2021). Rewriting the Microaggression Narrative: enhancing Nursing Students’ Ability to Respond. Nurse Educ. 46(2): 96-100. doi: 1097/NNE.0000000000000850.
- Johnson, V.E., Nadal, K. L., Gina Sissoko, D. R., & King, R. (2021). “It’s Not in Your Head”: Gaslighting, ‘Splaining, Victim Blaming, and Other Harmful Reactions to Perspectives on Psychological Science. 16(5): 1024 – 1036. doi:10.1177/17456916211011963
- Pusey-Reid, E., Gona, C.M., Lussier-Duynstee, P., & Gall, G. (2022). Microaggressions: Black students’ experiences – A qualitative study. Journal of Professional Nursing. 40: 73-78.
- Turner, J., Higgins, R., & Childs, E. Microaggression and Implicit Bias. (2021). The American Surgeon. 87(11): 1727 – 1731. doi: 10.1177/00031348211023418.
- Williams, M.T. Microaggressions Are a Form of Aggression. (2021). Behavior Therapy. 709-719.
Healthcare Disparities within Hospice Care
 Amanda Camden, BSN, RN
Amanda Camden, BSN, RN

Background
Hospice care entails caring for individuals with a terminal illness at their place of residence. The use of hospice care in the United States is increasing; however, racial disparities during end-of-life care still remain (Ornstein et al., 2020). For example, Black patients receiving end-of-life care often get more aggressive and potentially non-beneficial treatments when compared to White patients (Dierfeldt et al., 2021). Black patients are more likely to experience emergency room admissions and to be mechanically ventilated even if their condition is likely irreversible (Dierfeldt et al., 2021). Problems with underrepresented populations utilizing hospice care are not new; in fact, this is a long-standing problem (Bazargan & Bazargan-Hejazi, 2021).
When reflecting upon the reasons for these inequities, one must consider the deep-rooted history of racism and discrimination in the United States. COVID-19 illuminated healthcare disparities between different racial groups. For example, during the pandemic, American Indian, Alaska Native, Black, and Latino individuals had higher rates of hospitalization and death when compared to White people (Yearby et al., 2022). Yet the problem goes far beyond this. Looking at healthcare policies and funds allocation is needed to begin understanding the problem (Yearby et al., 2022). White people are more likely to be covered by employee-sponsored insurance programs, while underrepresented people (including Black people) are more likely to have low-wage jobs that do not provide adequate health insurance coverage (Yearby et al., 2022). Low-income workers who do not have adequate health insurance coverage are often not eligible for Medicaid or federal subsidies for health insurance; they often fall into a “coverage gap” (Yearby et al., 2022). Inadequate or non-existent health insurance coverage translates to an inability to pay for healthcare, including hospice care.
Referral Delays
Racial disparities in hospice care stretch farther than uninsured or underinsured rates. Another potential problem is the delay in referral time connecting patients to hospice providers (Bazargan & Bazargan-Hejazi, 2021). Delays in hospice referrals are greater in non-Hispanic blacks when compared to non-Hispanic whites (Bazargan & Bazargan-Hejazi, 2021). Other problems include cultural values that might conflict with hospice philosophy, lack of awareness regarding hospice services, and mistrust in the healthcare system (Bazargan & Bazargan-Hejazi, 2021). A multifaceted approach aimed at community partnerships and exploration of culturally sensitive interventions is needed to enable hospice care for all people, no matter the color of their skin.
Why Hospice Care Matters
Inadequate access to hospice and palliative care services results in adverse experiences such as more pain, more financial distress, and greater caregiver burden (Wachterman & Sommers, 2021). Additionally, hospice care can enhance the quality of life for individuals who have a terminal illness and also decrease Medicare costs (Ornstein et al., 2020). Some individuals would prefer to spend their last days at home, surrounded by family and friends. Hospice care can help facilitate this situation and can support families, too. Now is the time to begin changes to rectify this problem.
Ways to Solve the Problem
Culturally-sensitive interventions are urgently needed to address healthcare disparities during end-of-life care (Bazargan & Bazargan-Hejazi, 2021). We have an ethical responsibility to support and facilitate accessibility to hospice care services for all who need it. The literature is clear, Black people in the United States do not have reasonable access to hospice services. These citizens need advocacy and change to enable the fair distribution of hospice care. To be effective, hospice care must incorporate culturally sensitive practices to overcome cultural barriers (Dierfeldt et al., 2021). Current survey instruments are not culturally appropriate and are likely inaccurate at capturing Black patients’ experiences and reservations regarding hospice care (Bazargan & Bazargan-Hejazi, 2021). Thus, a culturally appropriate survey tool should be crafted and administered seeking to identify barriers to Black patients when they consider hospice care services. The Centers for Medicare & Medicaid Services (CMS) is a federal agency that provides health coverage through various programs (CMS - About Us 2023). The Office of Minority Health (OMH) is an entity within CMS that focuses on the integration of health equity in CMS’s policies and programs (The Centers for Medicare & Medicaid Services Office of Minority Health 2023). These federal agencies can help facilitate meaningful change, including the creation of an appropriate survey tool and linkages between hospice agencies and healthcare providers. Individuals should contact their state representatives and ask them to support legislation that will help remove racial barriers to healthcare access, including hospice care. Everyone, no matter the color of their skin deserves the opportunity to use hospice care if they so choose. It is the responsibility of those in power to enact changes that will facilitate the fair use of hospice services.
Article references
Bazargan, M., & Bazargan-Hejazi, S. (2021). Disparities in palliative and hospice care and completion of advance care planning and directives among non-Hispanic blacks: A scoping review of recent literature American Journal of Hospice and Palliative Medicine 38(6), 688-718. https://doi.org/10.1177/1049909120966585
The Centers for Medicare & Medicaid Services Office of Minority Health (2023). https://www.cms.gov/priorities/health-equity/minority-health/about/mission-vision-work
CMS - About Us (2023). https://www.cms.gov/about-cms
Dierfeldt, D., Knopf, K., & Jackson, L. (2021). Racial disparities at the end of life. American Family Physician 104(4), 346-247. https://www.aafp.org/pubs/afp/issues/2021/1000/p346.html
Ornstein, K., Roth, D., Huang, J., Levitan, E., Rhodes, J., Fabious, C., Stafford, M., & Sheehan, O. (2020). Evaluation of racial disparities in hospice use and end-of-life treatment intensity in the REGARDS cohort. JAMA Network Open 3(8). https://doi.org/10.1001/jamanetworkopen.2020.14639
Wachterman, M., & Sommers, B. (2021). Dying poor in the US - Disparities in end-of-life care JAMA Network Open,325(5), 423-424. https://doi.org/10.1001/jama.2020.26162
Yearby, R., Clark, B., & Figeroa, J. (2022). Structural racism in historical and modern US health care policy Health Affairs, 41(2). https://doi.org/10.1377/hlthaff.2021.01466
Consumer Utilization of Technology in Healthcare: Exploring the Role of the Nurse
 Lacey Cross, Cross, DNP, FNP-BC, CPN
Lacey Cross, Cross, DNP, FNP-BC, CPN

The role of technology in supplying consumer information in the healthcare sphere has expanded significantly over the past two decades. Finney Rutten (2019) and colleagues reported that in 2008, approximately 61% of adults reported seeking health information online as their first method to gather information. By 2017, that percentage increased to nearly 75% (Finney Rutten et al., 2019). Unfortunately, as the availability of health information has exploded with the advancement of technology, so too has the use and abuse of technology to promote misinformation and disinformation in the healthcare space (Basch et al., 2021). This article explores the role of technology in fulfilling consumers’ healthcare information needs and the role of nurses in promoting the safe use of technology by consumers in healthcare, specifically in the context of mitigating misinformation related to the COVID-19 vaccine.
Technology: Consumer Use and Abuse
The COVID-19 pandemic highlighted consumers’ reliance on technology as a source of health information in ways unrealized prior to 2020 (Yap et al., 2021). The internet played a key role in consumers’ ability to garner information during a time when other non-digital information sources were nearly inaccessible. The COVID-19 pandemic illuminated ways that technology could be leveraged for good through avenues such as telehealth. Unfortunately, however, we also learned of a darker side of technology during the pandemic and will be dealing with the related implications for years to come.
The development and authorization of COVID-19 vaccines were met with a surprising volume of resistance from many who expressed fear about the vaccine’s safety. Muric and colleagues (2021) collected data related to COVID-19 vaccine hesitancy, specifically within the Twitter social media platform. Nine of the ten (10) most tweeted URLs linking to vaccine information in their sample of 1.8 million tweets containing vaccine hesitancy content were links to sites determined to have low credibility (Muric et al., 2021). A study exploring the use of the TikTok platform found that among 100 trending videos related to COVID-19 vaccination, a slightly larger number of videos discouraging vaccination emerged than videos encouraging vaccination (Basch et al., 2021). Of the 38 videos discouraging vaccination, 26 contained content that parodied adverse reactions even prior to the vaccine’s initial distribution (Basch et al., 2021).
These examples represent the way in which technology can promote consumer misinformation, which is the spread of information based on incorrect facts (Basch et al., 2021). Measuring the impact of misinformation on the uptake of the COVID-19 vaccine is challenging, but these examples suggest that vaccination rates may have been affected by social-media-driven consumer misinformation. While conclusions cannot be made as to whether social media-driven misinformation is the cause of vaccine hesitancy, it has become clear that social media platforms may serve as drivers of misinformation acceptance and lower vaccination rates (Basch et al., 2021).
The Nurse’s Role in Consumer Protection
The role of the nurse in the technology space is similar to the role of the nurse in any patient care setting: to protect and promote patient safety. Although nurses have limited power to regulate the information that is disseminated through technological platforms, especially social media, there are actions we can take to mitigate the spread of misinformation and its effects on consumers. Specifically with regard to vaccines, healthcare providers are the most trusted source of information (Jones & James, 2021). Nurses should embrace the trust that the general public has placed in them, especially in the context of the significant uncertainty promulgated by misinformation on social media. This might look like efforts toward debunking any misconceptions patients hold after they have been exposed to misinformation.
Alternatively, nurses could also play a pre-emptive role by promoting factual information on their personal social media platforms (Jones & James, 2021). Furthermore, nurses could engage in “pre-bunking,” a strategy to address misinformation before it has the chance to become widespread (Jones & James, 2021). Ultimately, education is the key to protecting consumers. Nurses bear a responsibility not only to correct misconceptions when they arise but also to educate patients about what reputable and trustworthy information looks like and where to find it.
Additionally, nurses can promote consumer protection related to technology utilization by seeking opportunities for advocacy in the policy sphere and pursuing roles in leadership, especially in the health informatics space. Moreover, nurses can play a role in pursuing and securing funding to support initiatives aimed at sharing credible information with the public about vaccines and other important healthcare topics as well. Such initiatives could take the form of developing educational modules for high school or collegiate general education curricula or perhaps creating digital content educating individuals about the best ways to seek credible information that could be distributed via public health departments.
Conclusion
The role of technology in supplying consumers with healthcare information is undeniable in the current era. Unfortunately, the dark side of technology and social media has entered the spotlight as a result of the COVID-19 pandemic. The events of the past four years have highlighted the role of the nurse in consumer protection. Ultimately, nurses bear a significant responsibility to facilitate responsible stewardship of technological resources for the benefit of the public, and this responsibility is likely to continue expanding in the coming decades.
Article references
Basch, C. H., Meleo-Erwin, A., Fera, J., Jaime, C., & Basch, C. E. (2021). A global pandemic in the time of viral memes: COVID-19 vaccine misinformation and disinformation on TikTok. Human Vaccines & Immunotherapeutics, 17(8), 2373-2377. https://doi.org/10.1080/21645515.2021.1894896
Finney Rutten, L. J., Blake, K. D., Greenberg-Worisek, A. J., Allen, S. V., Moser, R. P., & Hesse, B. W. (2019). Online health information seeing among US adults: Measuring progress toward a Healthy People 2020 objective. Public Health Reports, 134(6), 617-625. https://doi.org/10.1177/0033354919874074
Jones, M., & James, J. (2021). Role of the nurse in addressing vaccine hesitancy and misinformation on social media. Nursing Standard, 36(12), 62-66. https://doi.org/10.7748/ns.2021.e11759
Muric, G., Wu. Y., Ferrara, E. (2021). COVID-19 vaccine hesitancy on social media: Building a public Twitter data set of antivaccine content, vaccine misinformation, and conspiracies. JMIR Public Health and Surveillance, 7(11), e30642. https://doi.org/10.2196/30642
Yap, S-F., Xu, Y., Tan, L. (2021). Coping with crisis: The paradox of technology and consumer vulnerability. International Journal of Consumer Studies, 24, 1239-1257. https://doi.org/10.1111/ijcs.12724
Part Of Your ANA/TNA Dues Is Tax Deductible!
You are allowed to deduct, as a professional/business expense, the percentage of dues that are NOT used by ANA or by TNA for political activities such as lobbying at the legislature. In 2024, the non-deductible percentage for ANA’s portion of the dues is 28.10%. The non-deductible percentage for TNA’s portion of the dues is 16.35%.
Deductible Amounts
Full-Premier ANA/TNA: $290 @ 55.55%--deduction $161.09
Full Standard ANA/TNA: $174 @ 55.55%--deduction $96.66
Bridging the Generational Gap in Nursing: How to Foster Collaboration
 Jennifer Hitt, PhD, RN, CNE
Jennifer Hitt, PhD, RN, CNE

In today's nursing workforce, it's common to find generations working side by side-Baby Boomers (1946–1964), Generation X (1965–1980), Millennials (1981–1996), and Generation Z (1997–2012). Each generation brings its unique perspectives, skills, and values shaped by the times in which they were raised. However, this diversity can also lead to challenges if not managed properly. Bridging the generational gap in the nursing workplace is essential to fostering collaboration, improving productivity, and maintaining a harmonious work environment.
Generational differences are often reflected in communication styles, work preferences, and technological comfort levels. Baby Boomers are often described as goal-oriented and competitive. Many prefer face-to-face meetings but are adapting to digital communication. Generation X is known for its independent, self-reliant nature. Members of this generation value work-life balance and are comfortable with both digital and traditional methods of communication. Millennials are characterized by their tech-savviness and desire for purpose in their work. They appreciate flexibility, collaboration, and feedback. Generation Z is the first fully digital-native generation. They value diversity, inclusion, and technology-driven communication. They often look for career growth and a strong alignment between personal values and work.
Understanding these general tendencies can help healthcare leaders and nursing colleagues navigate workplace dynamics more effectively. One of the most effective ways to bridge the gap is through clear and open communication. Encourage dialogue where nurses feel comfortable sharing their perspectives and ideas, regardless of their age or role. Creating open channels of communication helps dismantle stereotypes and fosters mutual understanding.
Pairing nurses from different generations in mentorship programs can be a powerful way to share knowledge and skills. For example, a Baby Boomer might mentor a younger nurse in nursing leadership, while a Millennial or Gen Z worker can help their older counterparts become more proficient in digital tools. Diverse, cross-generational teams are more innovative and productive. When designing teams or creating schedules, include nurses from various age groups to leverage their unique strengths. This not only enhances collaboration but also encourages a broader range of ideas and solutions.
Each generation has its own preferences for work-life balance. Offering flexible work arrangements, such as remote work or adjustable hours, can meet the diverse needs of younger nurses. Millennials and Gen Z often appreciate flexibility, while Boomers and Traditionalists may prefer structured schedules. Accommodating these preferences can improve job satisfaction across generations.
Generations have different preferences when it comes to communication. While Baby Boomers and Traditionalists might favor phone calls or in-person meetings, Millennials and Gen Z often prefer digital communication like email, instant messaging, or video calls. Offering a mix of communication channels ensures that everyone stays connected in ways that suit them best.
Offering training and professional development opportunities is crucial for all generations. However, ensure that the content is accessible to different learning styles. For instance, younger nurses may prefer on-demand, tech-based learning modules, while older nurses might appreciate more traditional formats, such as workshops or in-person training. A workplace that values diversity and inclusion will naturally do better at bridging generational gaps. Celebrating each employee's unique contributions helps foster a sense of belonging and respect. Leadership should encourage diverse opinions, challenge stereotypes, and create a culture where everyone feels valued.
Bridging the generational gap in the nursing workplace isn't about erasing differences—it's about embracing them. By fostering open communication, promoting mentorship, respecting individual work styles, and focusing on shared goals, nurses can harness the strengths of all generations. In doing so, they create a more dynamic, innovative, and productive work environment.
District News
District 1
 Charlotte Isabel, District 1 President
Charlotte Isabel, District 1 President

We’ve had an exciting quarter! We celebrated Nurses’ Week and recognized our most seasoned nurse, Nurse Weston for dedicating 54 years to the nursing profession. We are inspired and encouraged by her commitment to the field.

Congratulations! Lisa Lucas, the Chief Certified Registered Nurse Anesthesiologist (CRNA) at the Memphis Veterans Affairs Medical Center (MVAMC), has been named the 2024 recipient of the Alice Magaw Outstanding Clinical Anesthesia Practitioner Award by the 62,000-member American Association of Nurse Anesthesiology (AANA).
Lucas became the 38th recipient of the award on Aug. 3 during the AANA’s Annual Congress in San Diego. Each year, the Alice Magaw Award recognizes the accomplishments of a CRNA who is directly involved in patient care and has made important contributions to the advancement of nurse anesthesia practice.
Unfortunately, we are mourning the loss of two District 1 members: Beverly Massey and Dee Blakney. We will continue to keep them in our thoughts are prayers during this time.

Dee Blakney

Beverly Massey
District 2
 Angela Heartherly, District 2 President
Angela Heartherly, District 2 President
Recently, members of the Professional Development Council at The University of Tennessee Medical Center presented a session on #HealthcareAdvocacy. The goal was to educate UT nurses on how to become engaged and advocate for our profession and our patients. Members of TNA invited to speak were Angela Heatherly, Mark M. Miller, and Laura Barry. Each speaker gave their advice on how to get started as an advocate and what is the best and most effective way to advocate.
TNA District 2 will have its next meeting on October 8. Stay tuned for the details about this event.

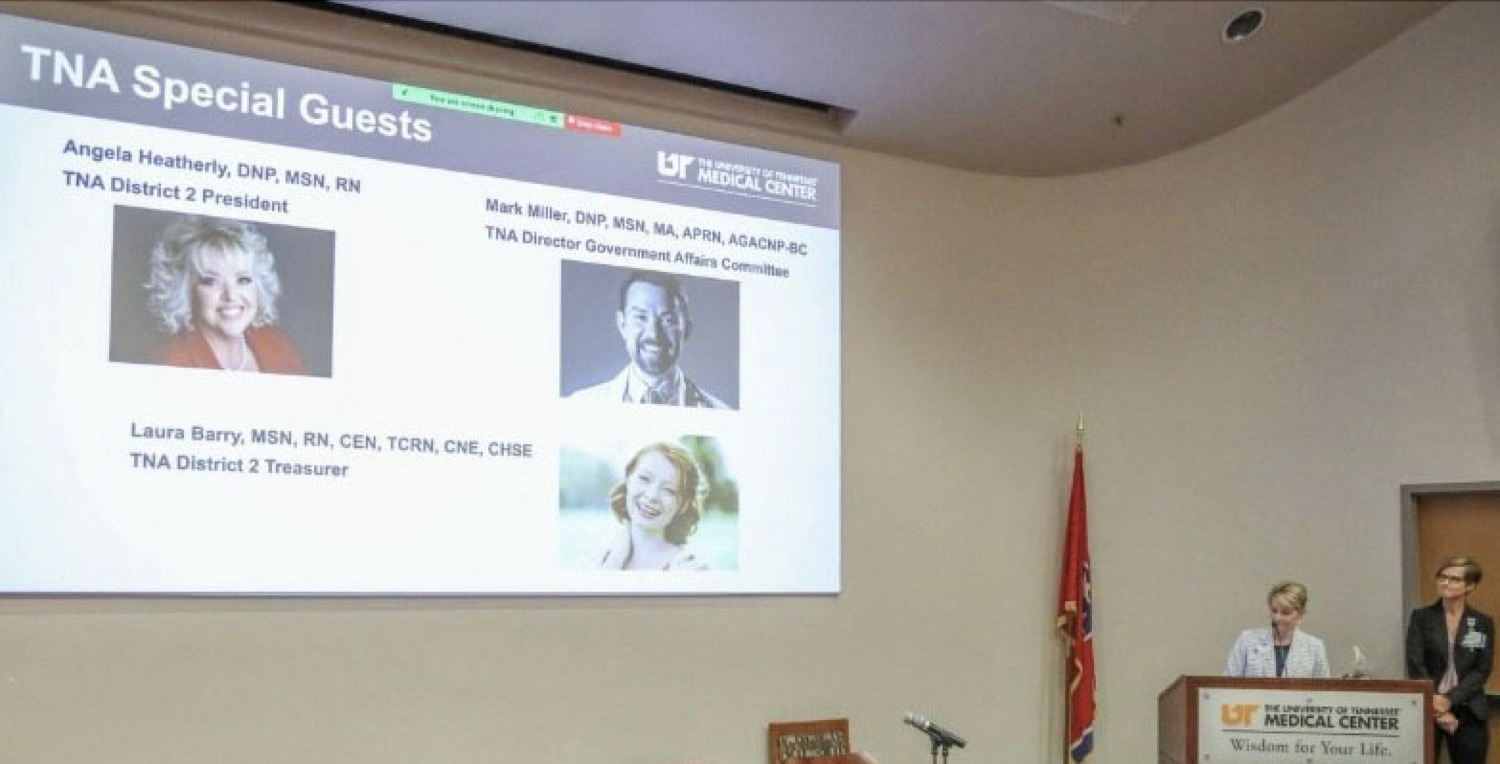
District 3
 Ashley Carter, MSN, RN, AMB-BC, CNEcl
Ashley Carter, MSN, RN, AMB-BC, CNEcl
July Membership Meeting: Virtual
On July 25, 2024, District 3 of the Tennessee Nurses Association hosted a virtual membership meeting with Garrett Johnson, the Chief Lobbyist for the Tennessee Nurses Association, presenting on "TNA Legislative Priorities and Updates." This insightful session provided valuable information on the current legislative landscape and priorities affecting nursing practice and healthcare in Tennessee. During the meeting, we also covered critical details regarding the upcoming elections, including key issues related to both general and local elections that are of particular importance to our nursing community. This discussion aimed to inform and prepare our members for the upcoming voting processes and to highlight the significant impact these elections will have on our profession and healthcare policies. Additionally, we were delighted to conduct a raffle during the meeting, offering one lucky member a complimentary registration fee for the upcoming TNA conference. This opportunity not only supports professional development but also encourages active participation in our association's events. Thank you to all who attended and contributed to the success of the meeting. Your engagement and commitment are vital to our continued efforts in advocating for nursing professionals and advancing healthcare standards in Tennessee. We look forward to your ongoing involvement and support.
District 3 Webpage:
Want to keep up with all the great things we're doing at District 3? Visit our district webpage to stay informed and engaged! Here, you'll discover valuable information about our current Board of Directors, upcoming meeting dates, access to meeting recordings, as well as details about exciting upcoming events and volunteer opportunities. Check us out, get active, and stay involved! Your participation and support make a difference in our community. Visit https://tnurses.care/District-3 today to stay connected and join us in making a positive impact!
District 3 Facebook Page:
We are immensely grateful to everyone who contributed to achieving our goal of 100 followers on social media in 2023! As we move forward into the new year, our aim is to connect with even more nurses, students, and community members. Your ongoing support is invaluable, and together, we look forward to expanding our online nursing community and making a positive impact in the year ahead. To locate our District 3 Facebook page, use this link: https://www.facebook.com/TNAD3MusicCityDistrict/. Please continue to help us spread the word by liking our posts, sharing them with your fellow nurses, and engaging with the incredible content.
District 3 Scholarship Update:
Are you a prelicensure or post-licensure nursing student in need of some funding for school? Be on the lookout for our District 3 scholarship opportunity. We are excited to announce that we plan to offer scholarships of $1,000 to one prelicensure student and one post-licensure student. Our scholarship subcommittee is deeply committed to helping students in District 3 achieve their educational goals. If you are interested in joining this subcommittee and contributing your voice to our efforts, we would love to hear from you.
Please stay tuned for more details on how to apply. We look forward to supporting you in your nursing journey.
Recognition of Nursing Students and New Nursing Graduates:
At District 3, we deeply value and support nursing students and are eager to see you join our ranks after graduation. We encourage you to consider joining the Tennessee Student Nurses Association (TSNA) in the meantime to benefit from the resources and networking opportunities it offers.
If you are a recent nursing graduate, we are thrilled about your achievement and would love to welcome you to District 3. Becoming a member of our district offers numerous professional growth opportunities, mentorship, and a community of dedicated nursing professionals. We look forward to your active participation and hope to see you soon!
Volunteer Opportunities:
District Elections will be held on October 24, 2024, at our quarterly membership meeting. All interested parties should submit their request to be added to the ballot or inquiries to district3@tnurses.care. Positions available include President-Elect, Vice-President, Secretary, and Director (2).
Your involvement can make a significant impact, and we welcome your interest in these positions. Together, we can make a difference in our community and profession.
Member News:
Congratulations to Director Cassandra Cassidy for recently being recognized by the Healthy Nurse Healthy Nation Blog Spotlight focus on “Shaping nursing students to create a healthier nursing profession.”

Congratulations to Dr. Susan Newbold for recently receiving the Ball State University (BSU) Nursing Lifetime Achievement Alumni Award. She is the first to receive this accolade. The award recognizes significant contributions to the profession of nursing and the BSU School of Nursing. She was presented with the award during the 2024 Alumni Association Reunion. Dr. Newbold is a November 1975 BSN graduate of the Muncie, IN. school and received the BSU Outstanding Nursing Alumni Award in 1995. She is an internationally known pioneer in nursing informatics. Susan and her husband live in Franklin, TN.
Congratulations to Michele Marbet, who was the lucky winner of the raffle for the TNA Annual Conference and Membership Assembly!
Congratulations to all the District 3 members who were selected for the 2024 Slate of Candidates for TNA at the state level:
- Mark Miller, DNP, MSN, MA, APRN, AGACNP-BC for President-Elect
- Sherry Raber, DNP, MMHC, MSN, RN for Vice President
- Jacqueline Buford, DNP, MSN, APRN-BC, RN for Vice President
- Tiffany Street, DNP, ACNP-BC for Vice President
- Julie Hamm, BSN, MSN, ACNP-BC for Treasurer
- Nancy Muldowney, DNP, RN, CHIE for Director of Education
- Daphny Peneza, MSN, RN, CNOR, CSSM, FAORN for Nominating Committee
District 4
 Brooke Epperson, District 4 President
Brooke Epperson, District 4 President
District 4 is doing well! Two DNP students presented their research at our last district membership meeting. This fall, we are planning some recruiting events at local facilities, and I hope to see many of our D4 members at TNA’s Annual Conference on October 10-12!
District 5
 Christine Reed, District 5 President
Christine Reed, District 5 President
Member News
Alicia Frasure, co-founder and member of TNA District 5, will soon open her own clinic.
Healing & Restorative Therapies (HART) is a new integrative mental health practice in the Tri-Cities area.
HART’s co-founders Alicia Frasure, FNP, PMHNP, and Rebecca Barger, LCSW, sought to create a mental health practice that is approachable, yet discreet, in order to help promote the mental health and emotional well-being of our clients. As a Women-owned practice, we welcome all gender identities and specialize in Women’s mental health issues across the lifespan. Our goal is to help bridge the gap in the mild/moderate mental health care needs in Tennessee and Virginia. HART offers counseling/therapy and medication management for mild/moderate mental health needs via telehealth or in office.
Alicia Frasure, FNP, PMHNP serves on the TNF Board of Trust and is Vice President of the Northeast Tennessee Nurse Practitioner Association.
Healing & Restorative Therapies will have an open house on Thursday, October 10, 2024, from 4:00pm to 7:00pm at 604 N. Roan Street, Suite 101 in Johnson City, TN.
Website www.hartheals.com
District 15
 Marcia Barnes, DNP, ACNP-BC, CWS, CPSN, TNA Chair-TN Nurses PAC
Marcia Barnes, DNP, ACNP-BC, CWS, CPSN, TNA Chair-TN Nurses PAC
Greetings from District 15!
District 15 held a meeting via Zoom on Monday, June 3rd. We were fortunate to have Kate Greer, MSSW, Director, Human and Trafficking Response Team. Kate works tirelessly with Ancora TN to nurture survivor healing and strategically combat human trafficking in Middle Tennessee. Through educating communities and professionals, Ancora TN works to stop human trafficking before it ever begins. She presented a very informative session with tips and warning signs for possible trafficking with each nursing encounter.
Our August meeting on the 5th was another success. We had the privilege of welcoming Marilyn Murry as the speaker for our Zoom meeting. She is an internationally recognized educator, theorist, author, columnist, and psychotherapist and is regarded as a pioneer regarding treatment of trauma. She has taught her Murray Method theory and treatment modalities since 1983. She shared with us her method as well as her experiences in Ukraine and Russia. The Murray Method presently has participants from over 310 cities in the former USSR, with Murray Method International Centers in Moscow, Russia; Poltava, Ukraine; and Dushanbe, Tajikistan. Very enlightening and informative session.
Congratulations and Kudos!!
Ken W. Edmisson, ND, EdD, RNC, FNP, CRNA, FNAP, is serving on the Poster Review Committee for the American Association of Nurse Anesthesiology for Fiscal Years 2023 and 2024.
Dr. Debra Rose Wilson orchestrated an article in the American Nurse with APSU colleagues Dr. Clark and Dr. Butler on the gut biome and health, which was published in April. Continuing Nurse Education article: https://www.myamericannurse.com/gut-microbiome-and-health
There is also a videotaped interview with the authors by ANA. Video: https://youtu.be/ms9W7Qpca4I
Dr. Debra Rose Wilson published in the August issue of American Nurse with APSU colleagues: Wilson, D. R., Pappas, J., & Taylor, R. (2024). Hypnosis and pain. American Nurse, 19(8), 35 – 39. Dr. Wilson was also inducted as a Distinguished Scholar with the Global Academy of Nursing.
Debra Sullivan, PhD, MSN, RN, CNE, COI, and colleagues have a recent publication: Sullivan, D., Hall, V., and Morrison, J. (2024). Navigating the future: Artificial intelligence's impact on transformational nurse leadership. Teaching and Learning in Nursing, 19(3), 298-300. https://doi.org/10.1016/j.teln.2024.04.017
Gina Haffner, DNP, FNP-BC, RN, Assistant Professor, Cumberland University School of Nursing, recently received the Frank and Oleda Rudy Endowed Professorship. Gina plans to use funds awarded to expose nursing students to health policy. These funds will aid in enhancing the curriculum within the policy program and facilitate bringing students to both the Tennessee and DC “on the hill” events.
Debra Sullivan, PhD, MSN, RN, CNE, COI, has had two articles accepted for publication in the Critical Care Nursing Clinics of North America: Pain Management 36.4: Sullivan, D. & Frazer, C. (2024). Navigating pediatric pain: Emerging trends and best practice and Bhatt, A., DeWitt, S. & Sullivan, D. (2024). Optimizing Patient Comfort: Palliative Pain Management for Nurses in Critical Care Settings. Debra also had three posters at the 2024 TNA conference titled:
- Sullivan, D. & Frazer, C. (October 2024). Transforming online nursing education through AI-powered learning.
- Sullivan, D. & Frazer, C. (October 2024). Empowering faculty and administrators: Leadership development in educational programs.
- Sullivan, D. & Frazer, C. (October 2024). Navigating pediatric pain Management: Integrating current guidelines for optimal care and clinical decision-making.
Dr. Mary Bess Griffith recently retired as Dean, Cumberland University School of Nursing after 51 years in the nursing profession! She will be missed for sure. Dr. Beth Chatham has been named the Director of the CU Nursing Program.
Deborah Lee, PhD, RN, NBC-HWC, NHC, Chair of Excellence in Nursing, and Director of the Positive Aging Consortium at Middle Tennessee State University School of Nursing, has been promoted to Professor.
Thanks to each of you for supporting and growing our profession with your scholarly endeavors.
Our remaining scheduled District meetings for 2024 are October 7th and December 2nd. More details coming. If you have suggestions for a speaker for one of our meetings, please reach out.
Kindly,
Marcia Barnes
District 15 President
Tennessee Nurses Foundation
Tennessee Nurses Foundation Board of Trust elects a new President, Treasurer, and Secretary.
Congratulations, Loretta Bond, Debra Sullivan, and Raven Wentworth, on your recent appointment as an officer on the Tennessee Nurses Foundation Board of Trust! For a complete list of the TNF Board of Trustees, visit TNurses.care and click on the TNF menu.
Photos Below Left to Right > Loretta Bond, Debra Sullivan, and Raven Wentworth


TNF Board Report
 Loretta Bond, PhD, MSN, RN, CNE -TNF President
Loretta Bond, PhD, MSN, RN, CNE -TNF President

I am Loretta Bond, the new president of the Tennessee Nurses Foundation (TNF). You might know me as the Vice President of the Tennessee Nurses Association. However, I am transitioning from the TNA Vice President role in October to serve as the new TNF President. I have been a member of the Tennessee Nurses Association since relocating to Nashville in 2015 from Wisconsin. Prior to that, I was an active member of the Wisconsin Nurses Association since graduation from nursing school. In practice, I have served as a nurse educator for 30 years. I also had my own clinical practice until 2019.
The Tennessee Nurses Foundation’s mission is to promote professional excellence in nursing. The goals are:
- Promote the professional image of nursing.
- Improve the professional and educational advancement of nurses.
- Facilitate leadership development.
- Encourage nursing research.
- Support professional health and wellness.
You will see programs from the Foundation that highlight these goals.
This is an exciting time for the Foundation as we prepare for the TNA Annual Conference on October 10-12, 2024. TNF, a major event sponsor, will hold its’ Annual Silent Auction fundraising event on Monday, September 30 – Saturday, October 12. The auction will be held online again this year, which was a great success last year. This is the link to TNF’s 2024 Silent Auction: https://tnfsa24.cbo.io. Click the link and register early as a bidder so you will be ready to bid on some fabulous items and excursions. Registering as a bidder is free, and you do not have to attend the conference to participate in the auction. The auction is open to everyone, so please share the auction link with your family and friends. Attendees at the conference will have an additional opportunity to purchase grab bags full of some great items and the foundation’s wine pull. The Silent Auction is TNF’s primary fundraiser for the year. Funds raised from this initiative help support the foundation’s scholarships, grants, and leadership fund. For more information on TNF’s scholarships and grants, visit TNurses.Care/TNF. We are currently accepting donations for the auction. Contact TNF@TNurses.Care for details.
Another TNF Initiative: As you drive around Tennessee, you will likely find yourself driving behind a car with a Nurses Change Lives license plate. We are happy to say that they are all over the state, and the foundation appreciates the support of everyone who has purchased the plate and is continuing to renew! If you haven’t purchased yours yet, you may have wondered what these plates represent. These plates, honoring Tennessee nurses, were designed by the Tennessee Nurses Foundation and approved by the Tennessee Legislature and the State of Tennessee Department of Revenue. TNF receives approximately one-half of your specialty plate cost, which helps support the initiatives I mentioned in the previous paragraph. When you purchase the specialty plate, you are supporting nursing here in Tennessee and sharing the important work that nurses perform with those who see your license plate. Drive with pride! Visit your local County Clerk’s Office to purchase your plate. It can be personalized for an additional fee.
TNF has a great group of Nurses and community members who serve the nurses of Tennessee, and we are proud and excited to support the work of the Tennessee Nurses Association.
TNF Fiscal Year 2023-2024 Scholarships, Grants, and Contest Announcements
The Tennessee Nurses Foundation congratulates our fiscal year scholarships and grants recipients! For a complete list of available scholarships and grants and to view those awarded, click HERE.
Thomas Apple’s manuscript, The Use of Nursing Research and Evidence-Based Practice Principles for the Development of a Compassionate Self-Reflection Tool Targeting Secondary Traumatic Stress Exposures won TNF’s 2024 Scholarly Writing contest. Thomas received $1,000 and a free registration to TNA’s Annual Conference on October 10-12 in Mt. Juliet, TN.
Healing Politics

Campaign School for Nurses & Midwives
Duke Sanford School of Public Policy
Durham, NC
June 5-8, 2024
Report by Courtney Nyange, Campaign School Participant, Recipient of the TNF Leadership Nursing Grant
My attendance at this remarkable, information-filled, and impactful campaign school would not have been possible without the support of the Tennessee Nurses Foundation. I am immensely grateful for the opportunity to have participated in the second annual Healing Politics Campaign School for Nurses & Midwives! From learning about the campaign process, to witnessing bipartisanship in action, to networking, this 4-day experience exceeded my expectations and increased my desire to run for elected office. I not only left the campaign school with concrete goals and an action plan to help me accomplish my goals, but I also left with the ability to articulate “my” why for running for office.
During my time at the campaign school, I learned a great deal about working with the media, developing a campaign plan and budget, fundraising, developing a communications and voter contact strategy, and how to help get out the vote. Most importantly, I connected with other nurses and legislators (also nurses) who share a common vision: making our voices heard and authentically representing the people. I am blown away by the compassion and dedication exhibited by my fellow cohort participants and left with so many lessons learned from them. I experienced a level of connectedness that has been hard to come by in this technologically enhanced world we are now living in.
Above, I mentioned that I left the campaign school with an ability to articulate my why. Here is my why for running for elected office: I believe it’s important for decision-makers to make decisions based on the values of the people they represent. I aim to bring diversity of thought, experience, and background to decision-making and be an advocate for solutions that are inclusive and equitable.
If you are at all interested in making a difference and are considering running for elected office, I encourage you to explore the Healing Politics Campaign School for Nurses and Midwives and get involved with our Tennessee Nurses Association political action committee (PAC) and/or our Government Affairs committee (GOVA). We need more nurses to run for office!
Advertise in This Newsletter
Nursing associations are among the most trusted partners in healthcare. Align your brand with our association to support us, deliver your message alongside editorial level content, build brand awareness, & reach our highly engaged / established audience.
For sponsorship rates and information within this official state nursing association publication, please contact Nursing Network at advertising@nursingnetwork.com
We appreciate your support!
Tennessee Nurses Association Board of Directors and Staff
|
TNA Board of Directors |
TNA Staff |
|
Jennifer Hitt, President Ray Coe, Past-President Tiffany Street, Vice President Julie Hamm, Treasurer Teresa Hobt-Bingham, Secretary Paula Walker, Director – Operations Nichole Knox, Director – Membership Christie Manasco, Director – Education Brett Young, Director – Government Affairs Belinda Fleming, Director – Practice Loretta Bond, TNF President-Ex-Officio |
Kirk W. Lawson, CAE, Executive Director Kathryn Denton, TNA Director of Operations, Managing Editor – Tennessee Nurse, TNF Program Manager Garrett Johnson, Director of Government Affairs and Chief Lobbyist Melanie Sain, Accountant |
Tennessee Nurses Association
545 Mainstream Drive, Suite 401
Nashville, TN 37228
Phone: 615-254-0350
Connect With Us