Nursing care is riddled with problems. Patient safety, new policies/regulations, performance benchmarking, patient satisfaction, incivility, and staffing shortages lead to concerns about providing high-quality patient care. These problems lead to workarounds, hacks, and corrective actions in search of explanations, remedies, and results—in other words, changes that will improve the quality of care we can provide within our work setting.
As a core pillar of our professional nursing education, we learned the nursing process: Assess, Diagnose, Plan, Implement, Evaluate (ADPIE). Systematically, nurses address individual patient problems and communicate the findings to others involved in the patient’s care. A Quality Improvement (QI) plan is initiated when addressing a problem within the caregiving system rather than developing a nursing care plan. Nurses instinctively participate in QI as an inborn nursing skill/trait. However, we need help to articulate it or share them with administrators.
Our brains are wired with a vast electrochemical, powerful micro-data-processing and transmitting system (Buzan & Buzan, 1993). This system is called radiant thinking and can be captured in a mind map (see Figure 1). According to Buzan and Buzan (1993), the radiant thinker (a brain-machine) has five major functions:
- Receiving - anything taken in by anyof your senses
- Holding - your memory, including retention
(storage) and recall (access)
- Analyzing - pattern-recognition and information-
processing
- Outputting - any form of communication or
creative act, INCLUDING thinking
- Controlling - refers to all mental and physical
functions (p. 36).
Table 1: Radiant Thinking Associated with ADPIE and PDSA Cycle
|
Major Functions
|
Receiving
|
Holding
|
Analyzing
|
Outputting
|
Controlling
|
|
Buzan & Buzan (1993)
|
X
|
X
|
X
|
X
|
X
|
|
ADPIE
|
Assess & Diagnose
|
Plan
|
Evaluate
|
Implement
|
QUALITY
|
|
|
|
|
|
|
|
QI
|
Plan
|
Plan
|
Study & Act
|
Do
|
Amazingly, we are wired for critical thinking and can utilize a mind-mapping technique to conduct ADPIE and PDSA Cycles for quality improvement.
An accurate definition of QI is “giving the people closest to the issues affecting quality of care the time, permission, skills, and resources needed to solve them.” (The Health Foundation, 2021). We have the skills, and nurses are great problem solvers, as evidenced by the numerous workarounds, hacks, and other methods designed to provide the best possible patient care within their particular care setting. Whenever a problem needs solving, nurses will brainstorm and devise a solution, implement the plan of action, tweak the plan as needed, and then share their successes (or failures) with others in an ongoing pursuit of the best possible solution. Both individual and overall patient care systems benefit from this problem-solving technique.
What patient care problems need solving in your unit, clinic, or facility? Are there new regulations or policies that require a change in the standard operating procedures? Is your hospital reaching for Magnetâ status or needing to maintain that status? What problems in patient care and patient safety keep you up at night? For what issues do you really wish you could help find a solution? What change would make your patient care setting a better place to work? These are the questions that drive the need for change, and QI projects are evidenced-based change projects designed to answer those questions and enhance patient care outcomes.
When developing a QI project, one method that correlates well with the nursing process is the Model for Improvement Plan-Do-Study-Act Method (PDSA). Once a problem is identified and possible solutions are considered, a Plan of action is developed and communicated to those who will be affected by the change proposed. (Assess, Diagnose, Plan). The plan is then implemented (Do) and tweaked as needed for a predetermined time (Study). Then, the outcome of the change is evaluated, and a decision is made to Act on the change. Since this is a cyclic process, the change can be adopted into the standard operating procedures of the care system or reenter any stage in the PDSA cycle. In all process stages, changes will continue to be implemented, evaluated, and adapted as needed to attain or maintain the desired results.
The ADPIE and QI processes share all the steps in determining quality based on the evidence (See Figure 1). Clinical facilities are encouraged to partner with their local graduate nursing schools to develop or update QI processes. The clinical facility gains a graduate student who is able to assist with the literature review under the guidance of their doctorate-prepared faculty advisor. The student may also be able to help lead in the implementation and summarization of the project, which are time-consuming for practicing clinicians. Additionally, the faculty gains access to real-world problems that reinforce the value of a DNP prepared nurse and guide the student in gaining competency in planning and leading changes within nursing practice.
Johns Hopkins Medicine offers a helpful worksheet to utilize when developing your QI project. It provides a framework for developing a Model for Improvement PDSA project which provides a framework for the project by answering three questions about the problem and then guiding the development of the change project into a validated method for evaluating change. (Institute for Healthcare Improvement, n. d). Of course, it is necessary to follow the guidelines for your facility’s Institutional Review Board (IRB) to ensure compliance and differentiate the QI project from a research initiative involving human subjects. The Department of Health and Human Services has a FAQ website that helps explain the rules regarding patient protection during quality improvement and research studies.
Model for Improvement PDSA as a QI initiative:
When developing a QI initiative, there should be a clear statement of the problem, the aim of the project, the specific measurements that will be used to evaluate the change, a summary of the findings, and the decision about incorporating the change.
Model for Improvement:
The purpose of the Model for Improvement is to help you clearly define what you hope to accomplish, how best to measure the outcomes, and what your literature search has helped you determine as the best evidence to use for your project. When developing these measurements, you will keep the SMART acronym in mind: Specific, Measurable, Achievable, Realistic, and Timely.
Problem Statement:
The problem statement should be a sentence or two that clearly states the problem: this is the current situation leading to this problem.
Aim Statement:
The aim statement clearly defines the goal of the change project. These goals should follow the SMART guidelines: Specific, Measurable, Achievable, Realistic, and Timely. To improve (your problem)-Specific from (current %) to (goal %)-Measurable, Attainable during (time of the project)-Time-bound for (setting in which the project will take place)-Relevant.
Example: To reduce the use of antibiotics from 25% to 10% over the next six months in adults with mild to moderate acute upper respiratory infections.
Example: To reduce falls from 25% to 10% over the next three months in patients (residents) identified as a high fall risk.
Summary of findings:
Once you have completed the PDSA cycle(s), the summary will compare your current outcome data to the baseline to determine if you reached your goal, then present the information to the QI team and other interested parties. At that meeting, a decision will be made about the proposed changes. Will the changes be adopted, adapted, or aborted? Will another change be studied?
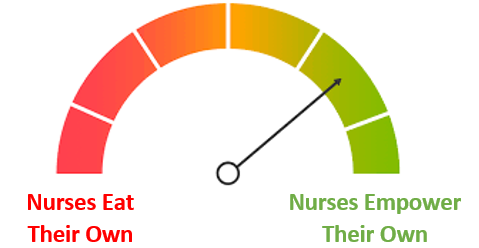
While QI projects are often seen as an administrative responsibility, nurses are often the people closest to the problems. Therefore, nurses are uniquely qualified to contact unit managers and nursing administration and offer their perspectives and solutions. As those closest to the problems, nurses can alert managers and administrators regarding developing issues. Together, administrators and nurses can then plan and implement a process to address them before they become problems. In an outpatient setting, the advanced practice nurse may wish to compare their performance outcomes to facility, state, and national benchmarks and then develop a QI plan to maintain or improve their patient care. Whether inpatient or outpatient, partnering with faculty in academia can enhance the project and promote collegial collaboration opportunities for faculty, students, administrators, and clinicians.
Nursing is the art and science of problem-solving. It is true in their individual patient care and in their desire to improve the policies and procedures that guide their patient care delivery system. Because nurses are experts in implementing the nursing process for solving patient care problems, they can translate those skills into addressing institutional patient care problems. As the ones closest to the problems, they are most qualified to help develop, implement, and evaluate the needed changes.
Now that you know how to formalize your workarounds and hacks, you can document your processes. The Model for Improvement Plan-Do-Study-Act (QI method) is like the nursing process and thus simple to adapt by nurses to communicate the plan in which to solve systemic patient care problems. Organizing the documentation of this process into a recognized QI method allows the nursing profession to share its successes with others as well as advise them of changes that did not provide the desired outcome. As a bonus, you now have the tools needed to develop a DNP project when you are ready to tackle that goal.