Happy spring Nurses of Georgia!
It has been a wonderful two years of growth, learning, and exciting change! We are in a time where it is essential that we lend our voices and spring into action! There are many milestones that we have seen together and legislation that has been enacted because of Our diligence.
However, the work continues. This Nurses' month let's make it count! The power of Nurses is being amplified through advocacy. Being the largest part of the healthcare mix, our voices hold weight. When we speak in unity, and when we allow our passion to be felt, policies change!
It has been my honor to be the chairwoman of the board of directors for the Georgia Nurses Association (GNA) for the past two years. In August, I will pass the torch to the very capable Dr. Joy King. She has been an unwavering support system for me in this role as well as an advocate for the Georgia Nurses Association in many roles. Joy, your hard work does not go unnoticed! I'm so grateful to have gained a nurse sister, friend for life.
I would like to take this time to thank the hard-working board of the GNA. Each of the directors hold their positions very dearly and take them seriously.
I am grateful to the awesome staff of the GNA. Thank you, Matt Caseman for being the best honorary nurse ever.
The incomparable relationship that the GNA holds with the Georgia Nurses Foundation makes it even better. To the outgoing president, Wanda Jones. Thank you for being a guiding force and inspiration to many. Wanda has been by my side through it all. It has been a sincere honor to work alongside of you and to have the wealth of knowledge that you have at my fingertips. Thank you, thank you and thank you!
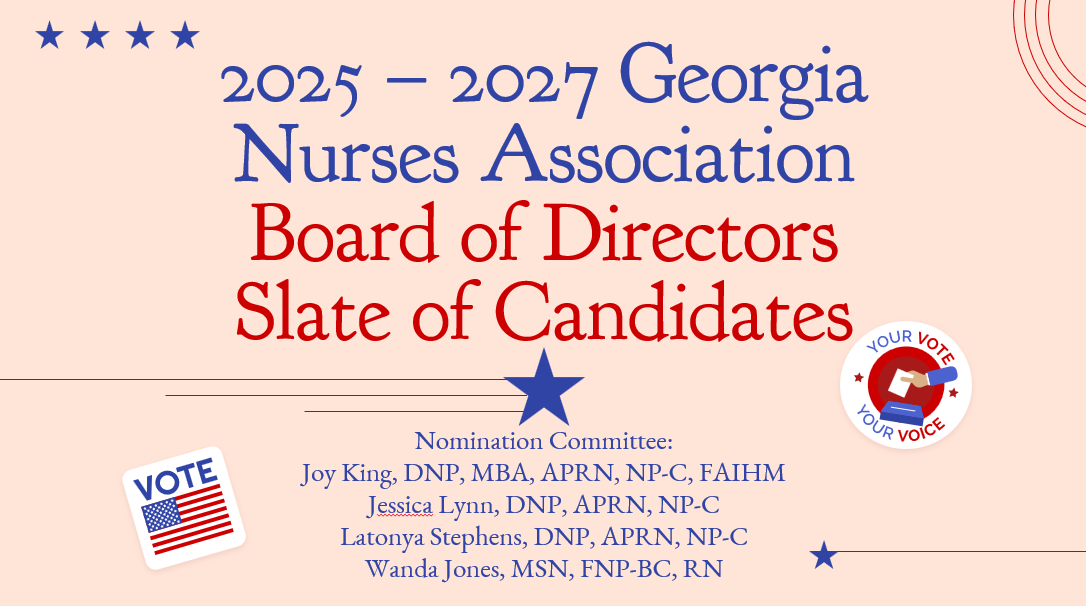
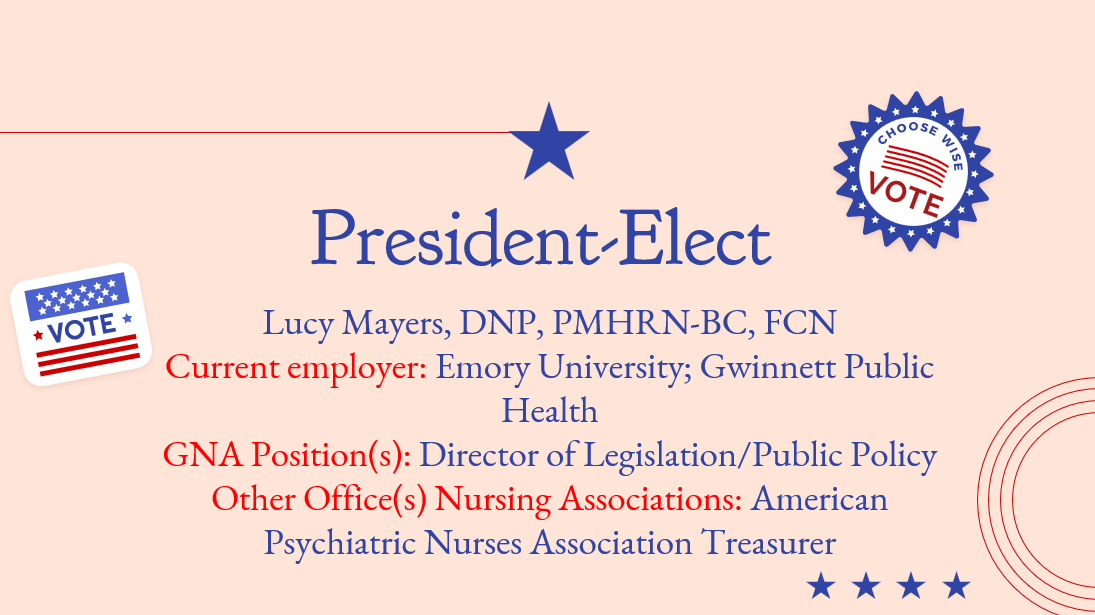
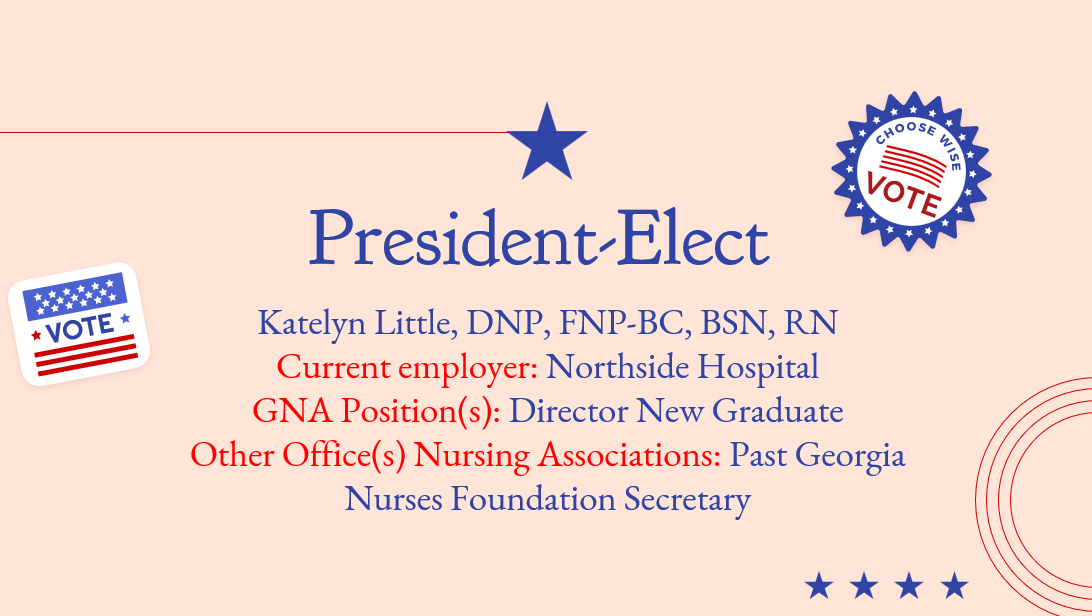
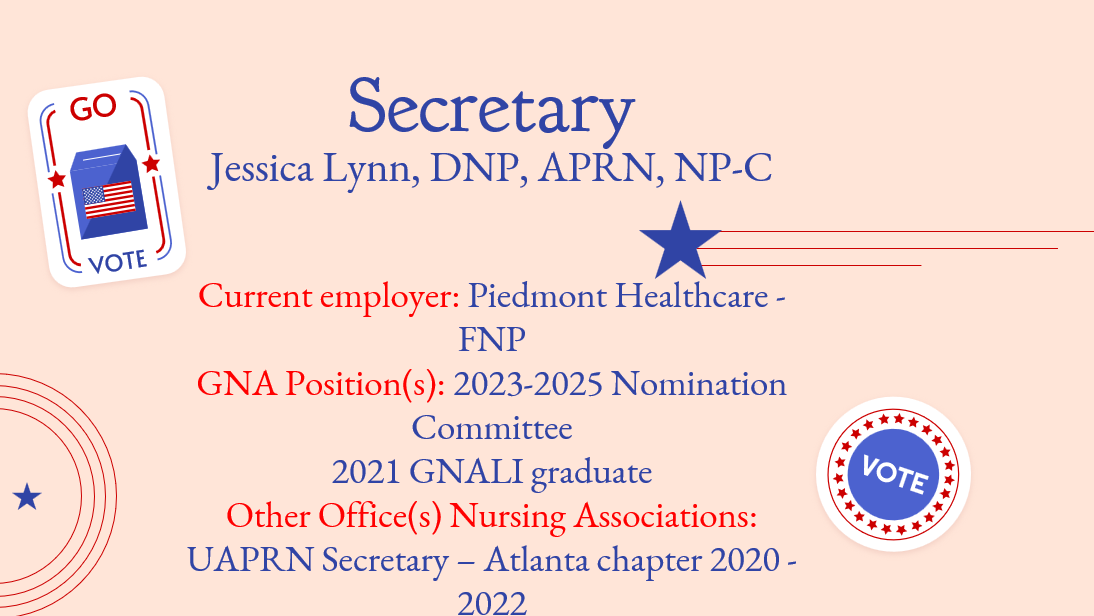
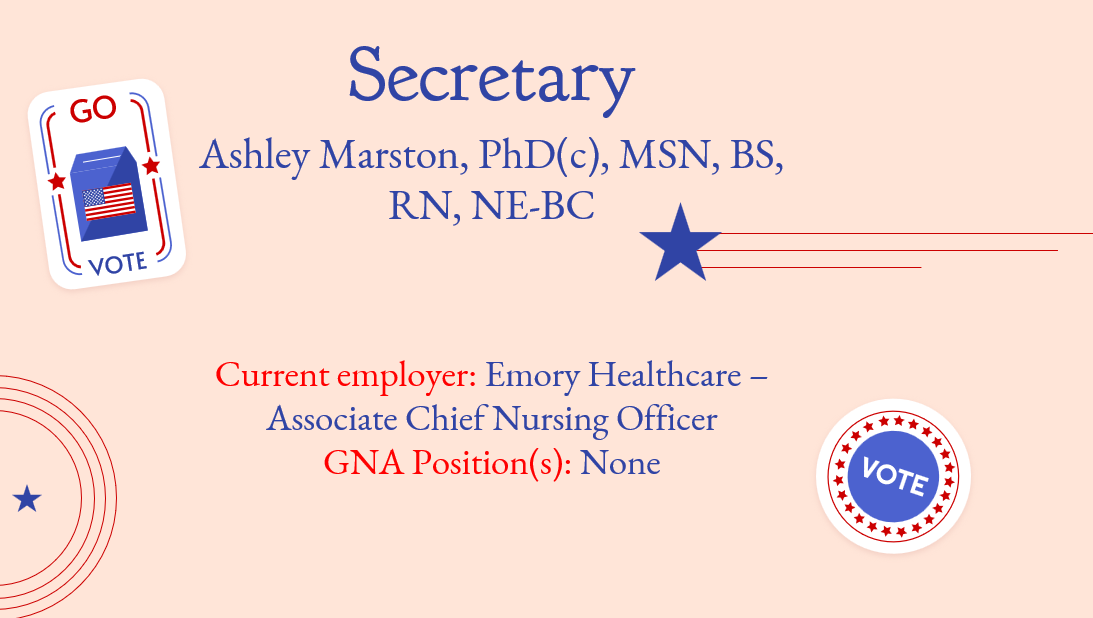
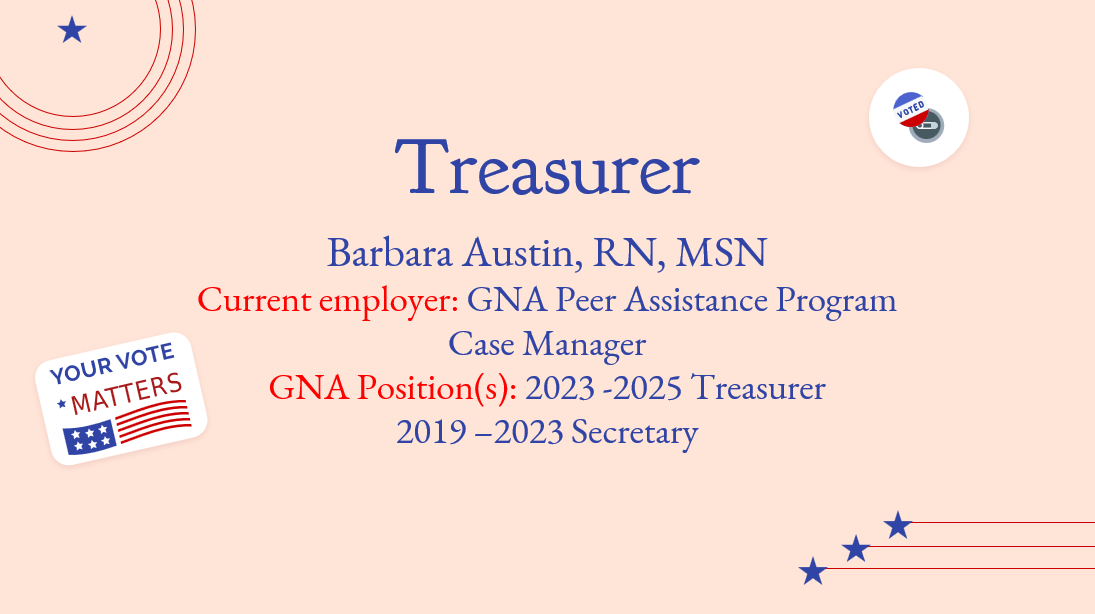
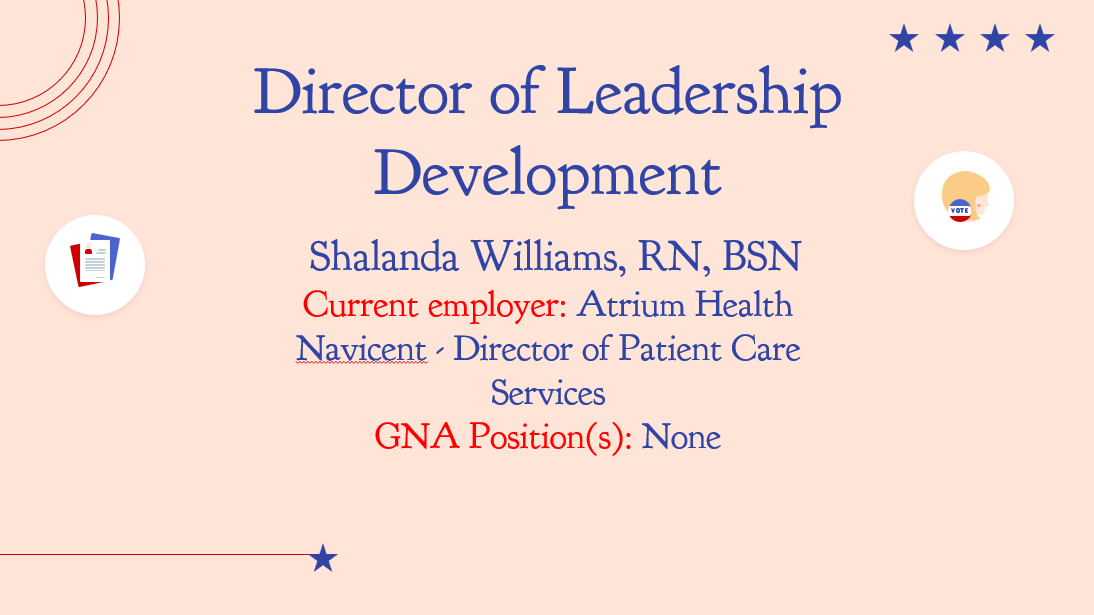
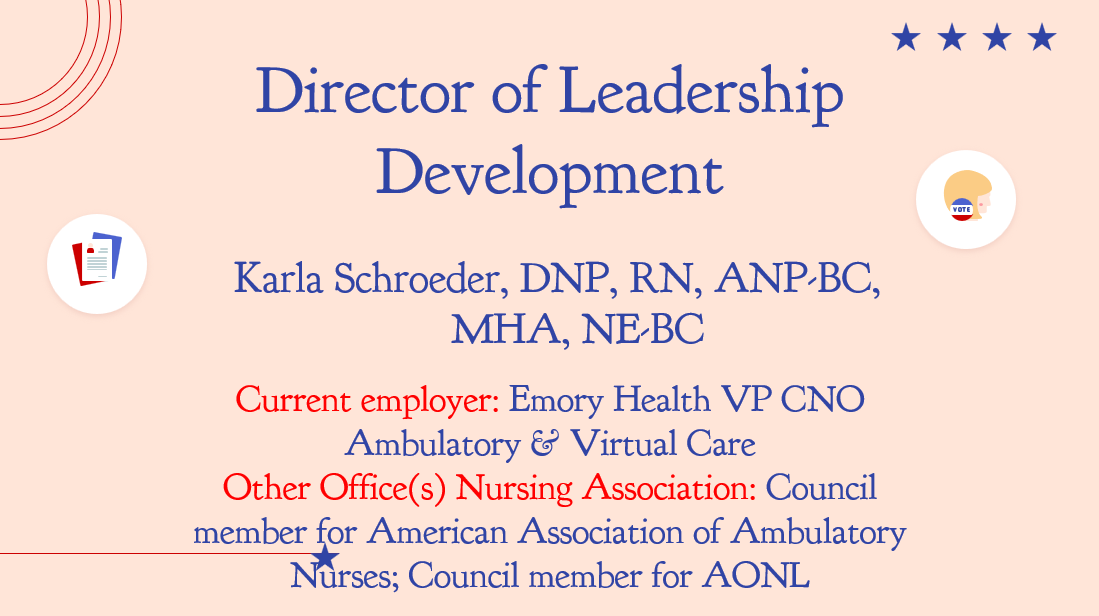
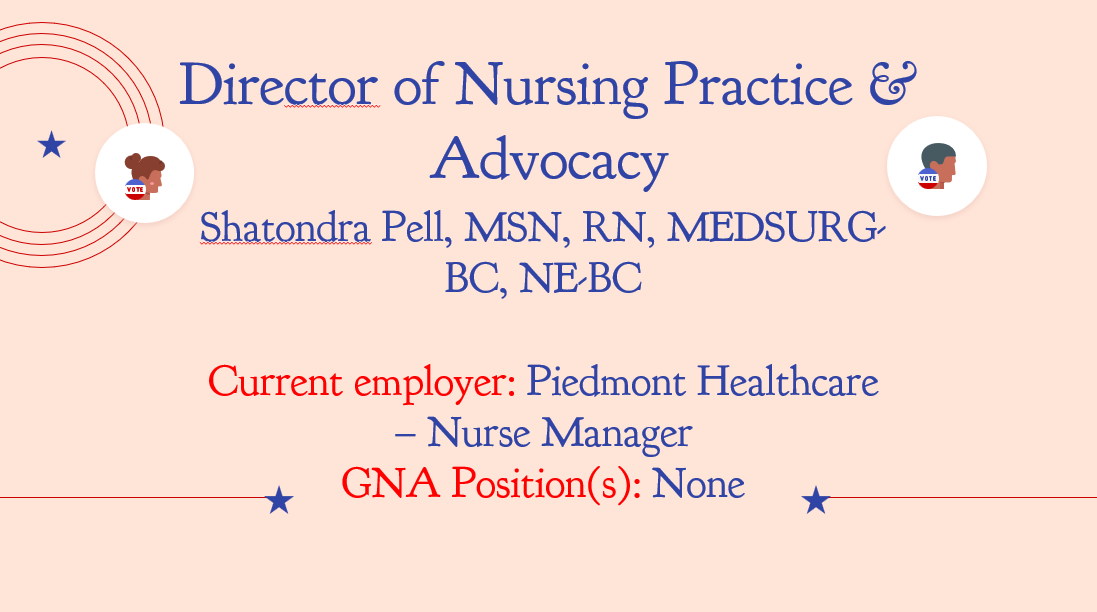
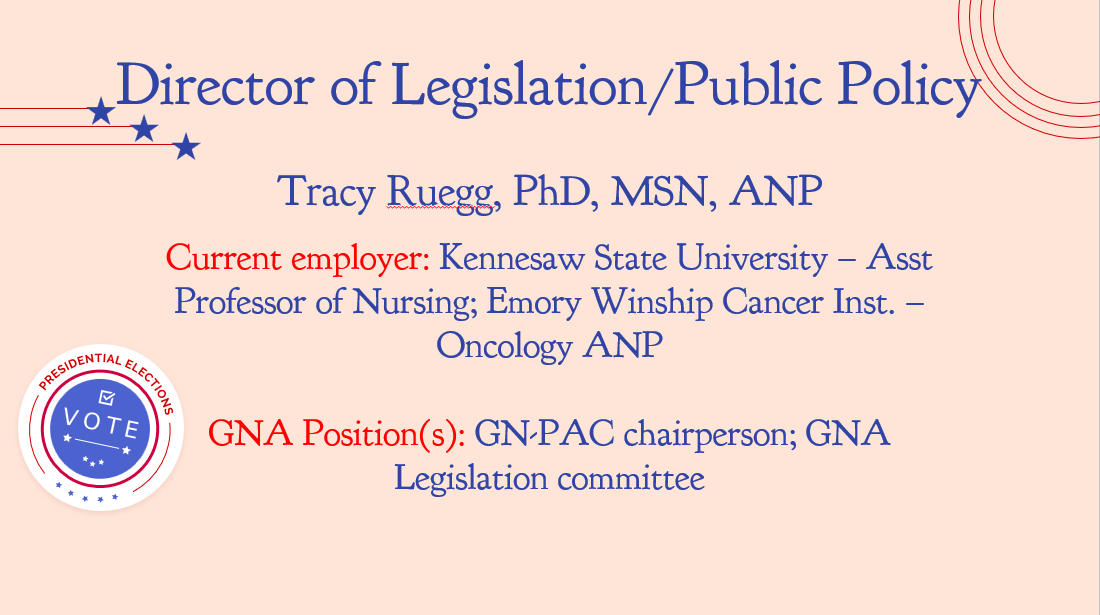
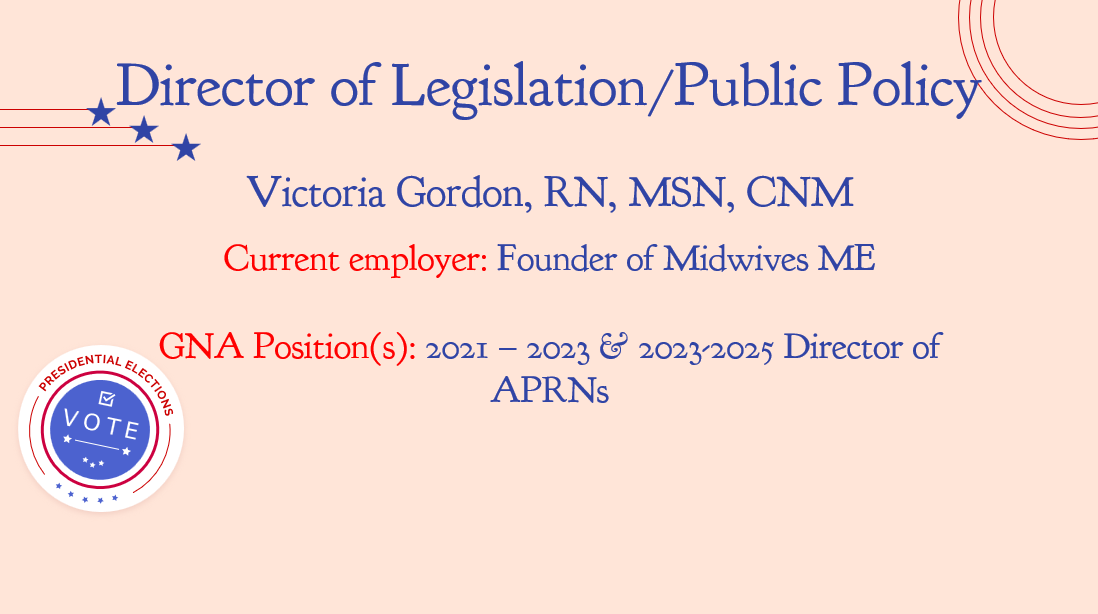
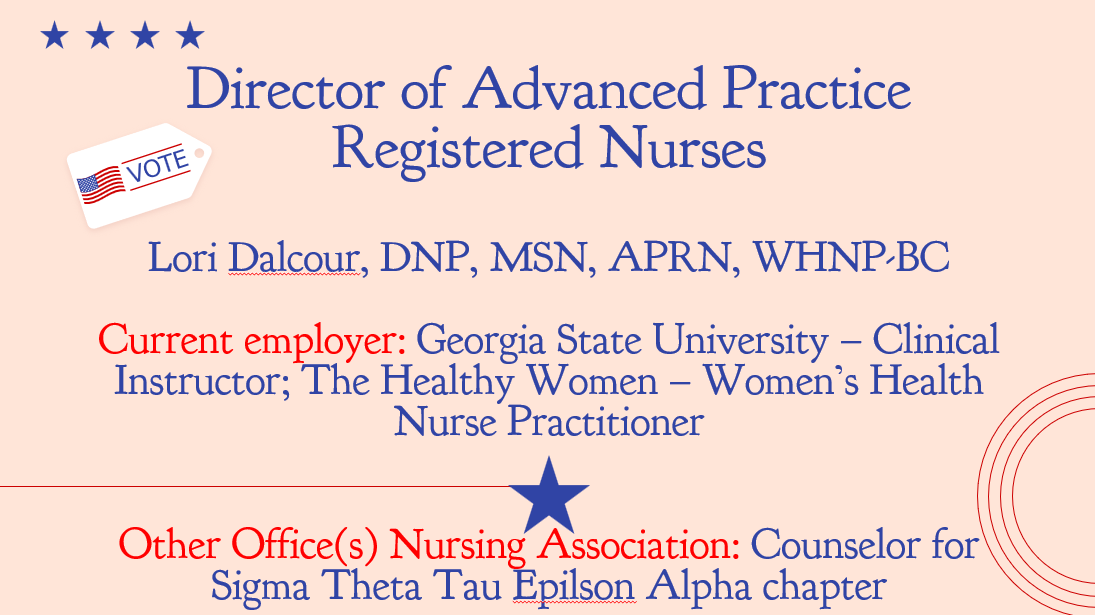
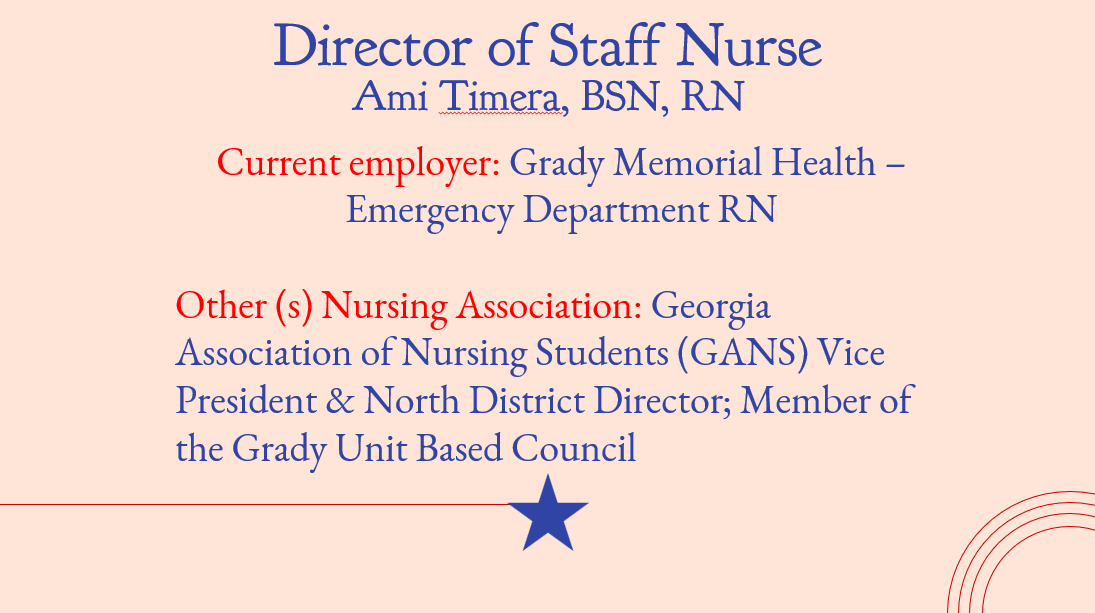
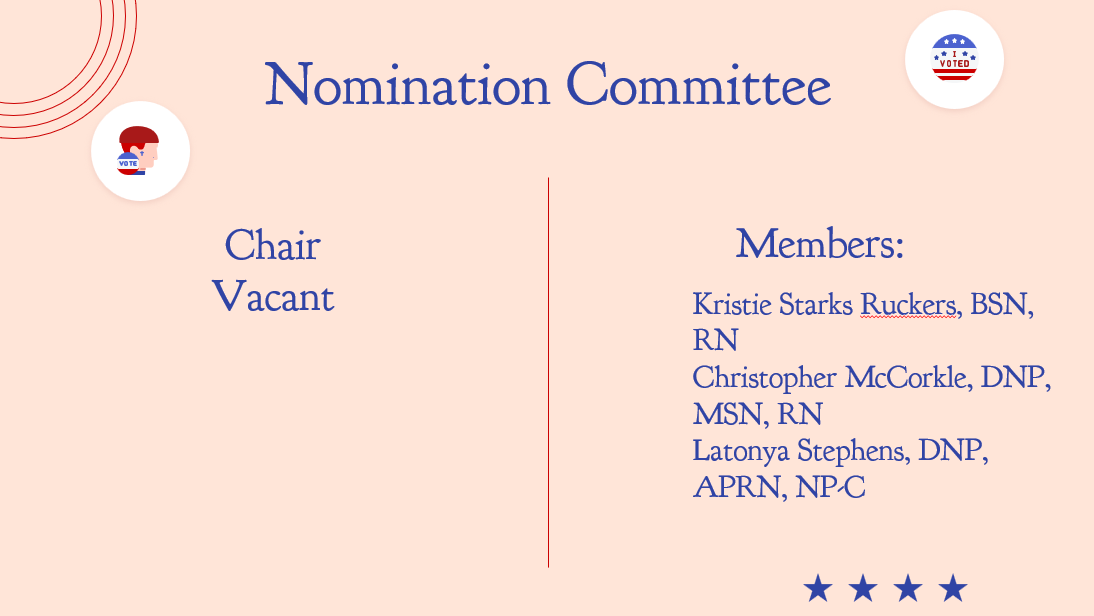
It is a great pleasure to welcome the new slate of candidates. Best wishes to each of you.
Voting is very important, and it is your civic duty. As a member of this organization, we ask that you consider exercising your right to be informed with each of the candidates and to vote accordingly.
I will continue to serve in the role as an advisor now that I have this experience under my belt. I have used many of my messages to the membership to not only express my gratitude for you all entrusting me in this role, but also for encouragement of self-care. I would be remiss if I did not continue along these lines by reminding you as spring comes into season that it is time to smell the roses. Stop and do those things that bring a smile to your face again.
It is ok to have fun and to do things that bring you happiness. Sometimes that involves going back to things that are primitive. I enjoy coloring because it takes your mind to a new place and it allows it to rest for a little bit.
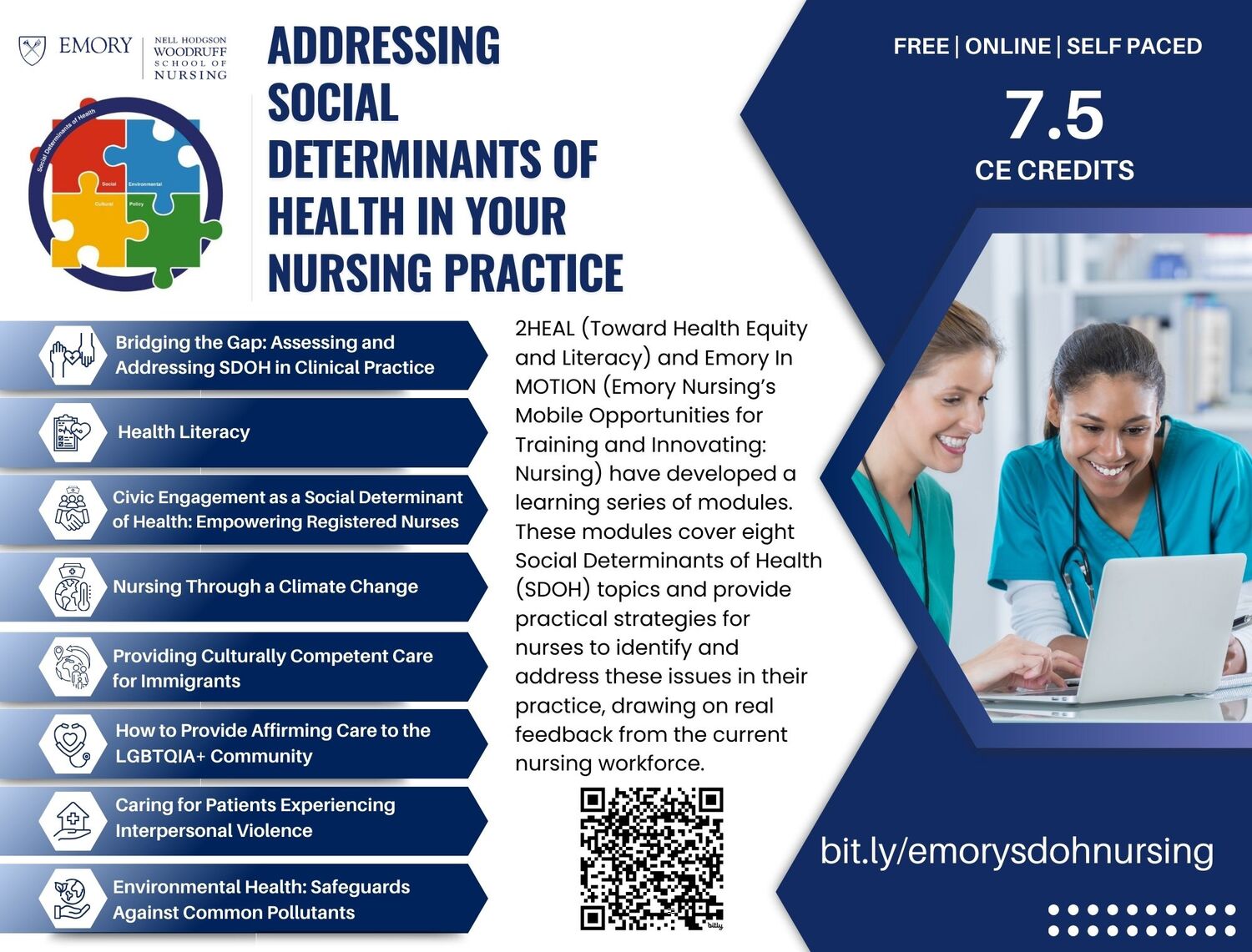
At the conference, August 22 through the 24th in Columbus, you will have the opportunity to not only continue your education but also to take part in exploring the beautiful city and all that it has to offer! The downtown area is quite scenic, filled with many restaurants and businesses that you can patronize. Also, there are several upcoming events posted by the GNA and partners that are listed on the website. Please look at the events page and join us as we gather and continue to work on our priorities.
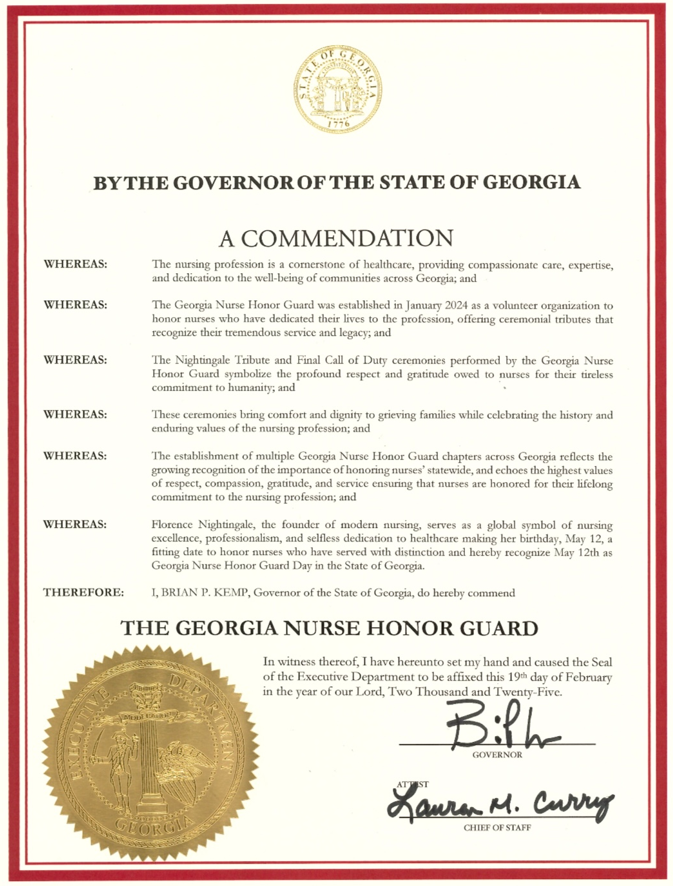
This 2025 legislative session was extremely fruitful. A huge thank you to GNA Senior Director of Membership & Government Affairs Tim Davis who works tirelessly alongside of our very reputable lobbyists. We have forged many great relationships under the gold dome, and it shows.
The summer months are a time where many families get together and do fun things. As you gather with your family and plan your downtime, remember that you have earned it and you deserve it!
There are many legislators who are nurse advocates, and huge supporters who are looking for opportunities to help remedy some of the less desirable situations that we find ourselves in. Become their trusted advisor. There is innovative work being done in the state of Georgia.
Although Georgia is currently ranked number seven in the nursing shortage, GNA is working feverishly to improve the practice environment for nurses. If you have any suggestions on ways that we can attract talent to help curtail this issue, we are here to listen. Nurses, THANK YOU for all that you do.
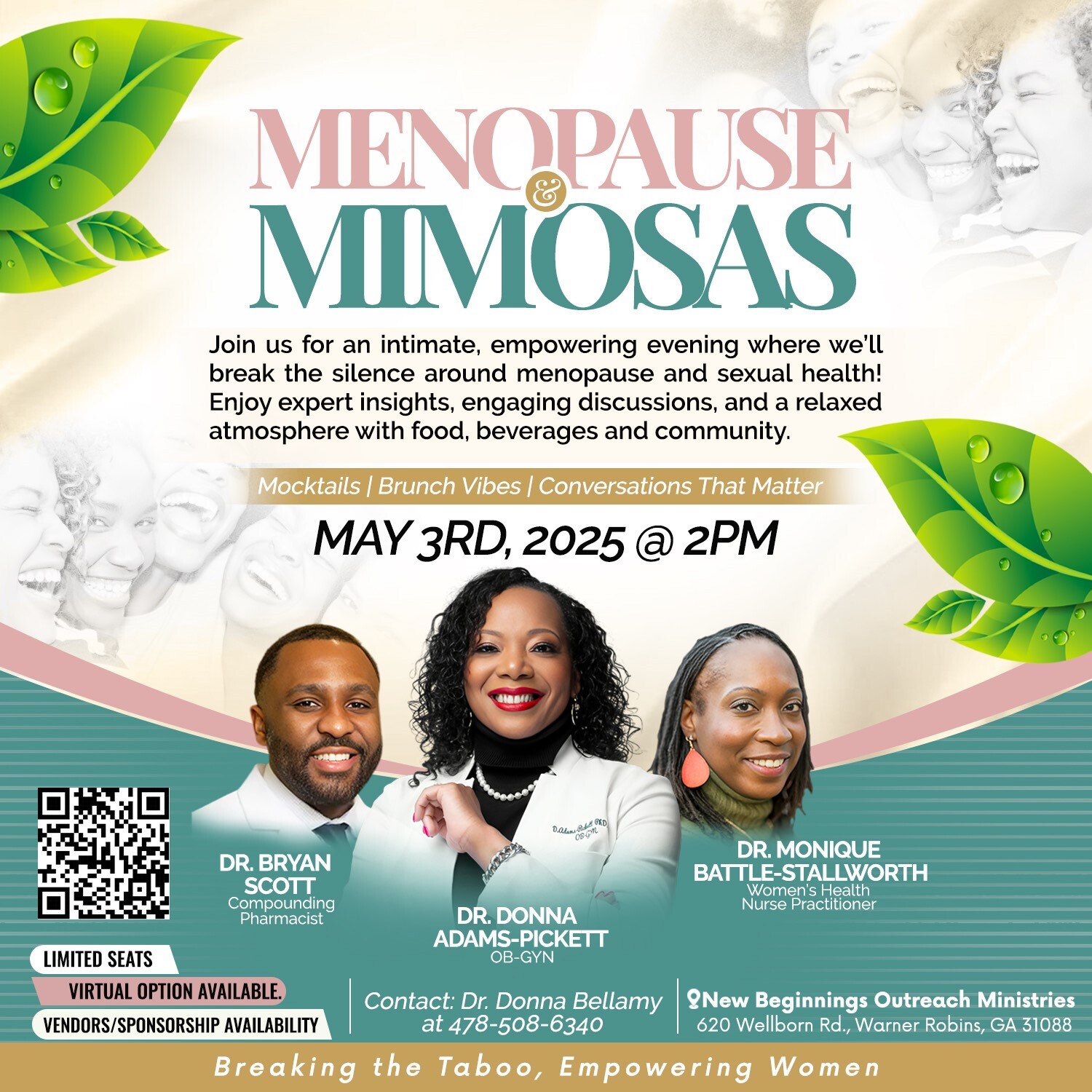
Allow me to be one of the first to tell you "happy nurses week" and happy national nurses month. We hope to celebrate with you at GNA Headquarters on May 3!
Please do not forget to celebrate yourself a little more this month and to recommit to the passion that brought you into our beloved profession!
Wishes of continued health to you and yours.
With immense gratitude, Erica Mills, PhD, RN, NPD-BC,
President, Georgia Nurses Association