Thank you for taking the time to read Nevada RNformation, the official publication of the Nevada Nurses Association (NNA). I thank the Editorial Board, who works hard to fill the quarterly issues each year with interesting and informative articles. Also included in each edition are updates on activities offered by NNA and the Nevada Nurses Foundation (NNF), which is NNA's philanthropic arm. So, please enjoy!
Nevada's Legislative Session: Stay Informed
The 83rd Nevada Legislative Session began on February 3, 2025. Now is when nurses can make a difference and communicate about the proposed legislation. All committee and session meetings can be viewed in person, virtually, or on your own time since meetings are recorded. Individuals can provide testimony on budgets and bills in Las Vegas, Carson City, or over the telephone. Visit www.leg.state.nv.us to find the following information: (1) Bill Draft Requests (BDR) filed, (2) information about committee meetings including the agenda, (3) Senate and Assembly session times along with the agenda, (4) information about the legislators, and (5) the ability to track 10 bills for free.
Nurse's Day at the Legislature -- May 20th
NNA hosts a Nurse's Day at the Legislature (NDAL) during the Legislative Session. This year's event will be held at the Capitol on May 20, 2025. Some nurses can sit on the Assembly or Senate Floor with their legislator and will be recognized and recorded in the Daily Journal. Additions this year include the requirement that attendees complete a 1 CEU course before the event. The goal is to have as many nurses attend as possible. Attend to hear from NNA's Lobbyist and learn about some bills that may impact nurses. Please visit NNA's website, www.nvnurses.org, or read the NNA Legislative Committee's article in this issue for more information about this event. Please join us and learn more about the legislative process or the bills that may impact nurses.
NNA's Conference -- Connect with Nurse Colleagues
Here is an opportunity for you to join nurse colleagues in addressing the issues and challenges facing the nursing profession in Nevada. I am so excited that NNA will be having a Conference that starts in the evening on Sunday, May 18, and continues on Monday, May 19, in Carson City. On Sunday evening, join the NNA Board for a silent auction, networking, and fun. Monday will start with breakfast and lead to some CEU presentations, including lunch and dinner. Six CEUs are available for full attendance. There will be some time in the afternoon to explore the area and join other nurses on a hike or visit a museum. The conference is the day before NDAL so that nurses can attend both events. However, you have the flexibility to participate in one or both events.
Some other in-person events will be planned by District 1 (Northern Nevada & rural) and District 3 (Southern Nevada) in the upcoming months. If you are not an NNA member but are receiving this publication, please join NNA on our website. As a member, you should receive the NNA's "Monthly E-News and Updates." If you are not receiving the e-mail, ensure NNA has your correct and preferred e-mail address.
Now, I want to tell you what the Nevada Nurses Foundation (NNF), the charitable and philanthropic arm of NNA, is working on for 2025. NNF holds fundraising events twice a year. Money raised provides scholarships to individuals seeking initial nursing education, advanced nursing education, or grants for furthering the nursing profession. The Margaret Curly Rural and Frontier Nursing Symposium is held twice a year. This event raises funds for the Rural and Frontier Nursing Scholarship.
Another NNF annual event is the themed Big Hat, High Tea, held at the Governor's Mansion in April. This event sells out, so get your tickets early at www.nvnursesfoundation.org. A ticket includes a delicious tea and lunch, a playful ambiance, an incredible silent auction, a fun live auction, and exciting raffle prizes. You can purchase raffle tickets for exciting prizes before and at the event. Approximately a month before the event, directions to buy tickets are on www. www.nvnursesfoundation.org. Silent auction prizes can be bid on before and during the event.
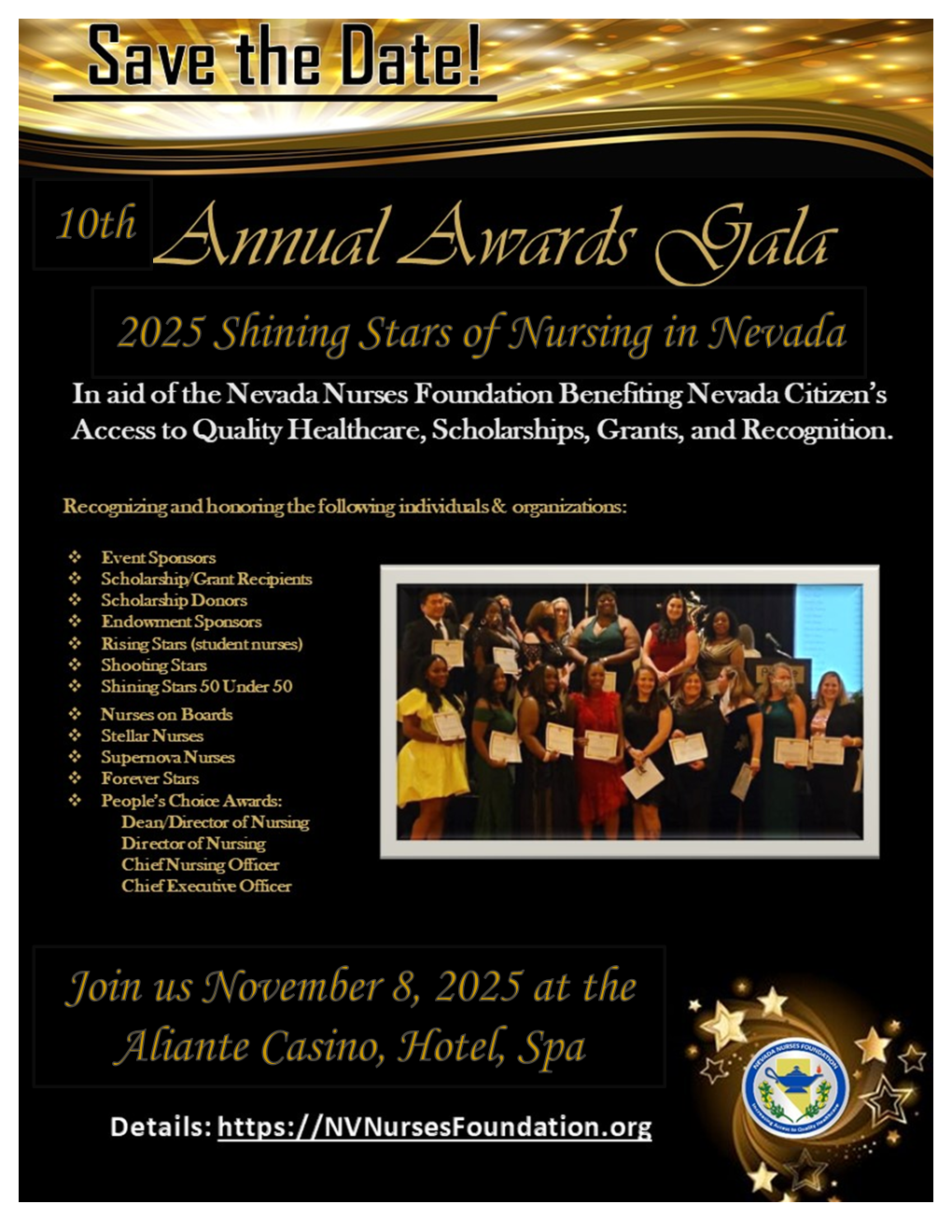
The Annual Shining Stars of Nursing Gala in October or early November is the significant event that wraps up the year. This event alternates between Las Vegas and Reno. The event this year will be at the Aliante Casino, Hotel, Spa on November 8, 2025. I invite you to join these events and help raise money for nursing scholarships. Please read the NNF Column in this issue, which has more information about the most recent Margaret Curley Rural and Frontier Nursing Symposium, scholarship applications, and more.
Promote professional nursing practice -- Join NNA!
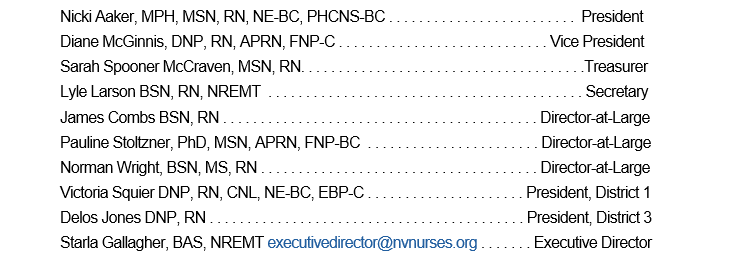
If you have questions about NNA, want to get involved, or have a general question, please e-mail NNA Executive Director Starla Gallagher at executive@nvnurses.org. She can assist you or ensure you are directed to the appropriate person. We are always looking for individuals to get involved, so please get in touch with us. I hope to meet many of you at one or more of our events in 2025.