From data to action
Strategies to achieve a sustainable nursing workforce
By American Nurses Association
In 2023, the Nurse Staffing Task Force, a collaboration between the
American Nurses Association (ANA) and the American Association of
Critical Care Nurses (AACN), an ANA organizational affiliate, outlined
five imperatives, 16 recommendations, and 65 associated actions to
actualize a sustainable nursing workforce. The five imperatives the Task
Force cited as essential to resolving the nurse staffing crisis include
reforming work environments, innovating care delivery models,
establishing staffing standards that ensure quality care, improving
regulatory efficiency, and valuing the unique contributions of
nurses.
In the fall of 2023, the Task Force hosted a free, five-part
interactive Project ECHO® webinar series to explore these proposed
initiatives. More than 2,800 individuals participated by listening to
featured Task Force member presentations and joining interactive, small
group discussions.
The recordings, presentation materials, and follow-up questions from
all five sessions are now available for anyone pursuing solutions to the
nurse staffing crisis (hubs.ly/Q02kMCmQ0).
The series opened with Linda Cassidy, PhD, APRN, CCNS, CCRN-K,
strategic advocacy manager at AACN, and Sarah Delgado, DNP, RN, ACNP,
clinical practice specialist in strategic advocacy at AACN, exploring
the imperative around reforming the work environment. Appropriate
staffing, they suggested, is inextricably linked to the health of the
work environment. Creating and sustaining a healthy work environment
requires deliberate effort. They added that leaders play an essential
role in this regard and must have support in doing so.
Healthy work environments, Cassidy and Delgado stressed, don't just
happen---they take deliberate commitment and action by leaders---and
have no finish line.
In the second session, Task Force members Vicki Good, DNP, RN, CENP,
CPPS, chief clinical officer of AACN, and Lesly Kelly, PhD, RN, FAAN,
scholar-in-residence for the Task Force, explored the value of nurses'
unique contributions to healthcare. In hospitals' pay-for-performance
models, various metrics track the value nurses add through direct
benefits, cost avoidance, and cost savings.
If all RNs had a unique nurse identifier, as recommended by the Task
Force, these data could be mined to quantify nurses' contributions via
assessments, interventions, and outcomes.
Good and Kelly also outlined the advantages of a formalized and
customizable organization-wide total compensation program, another Task
Force recommendation. They described six actions that organizations
might consider, such as implementing creative compensation for
hard-to-fill shifts.
In Session 3, presented by Kiersten Henry, DNP, ACNP-BC, CCNS,
CCRN-CMC, chief advanced practice provider at MedStar Montgomery Medical
Center, and Katie Boston-Leary, PhD, MBA, MHA, RN, NEA-BC, director of
nursing programs at ANA, considered how innovative care delivery models
could improve patient and nurse satisfaction, reduce practice pain
points, and yield better outcomes.
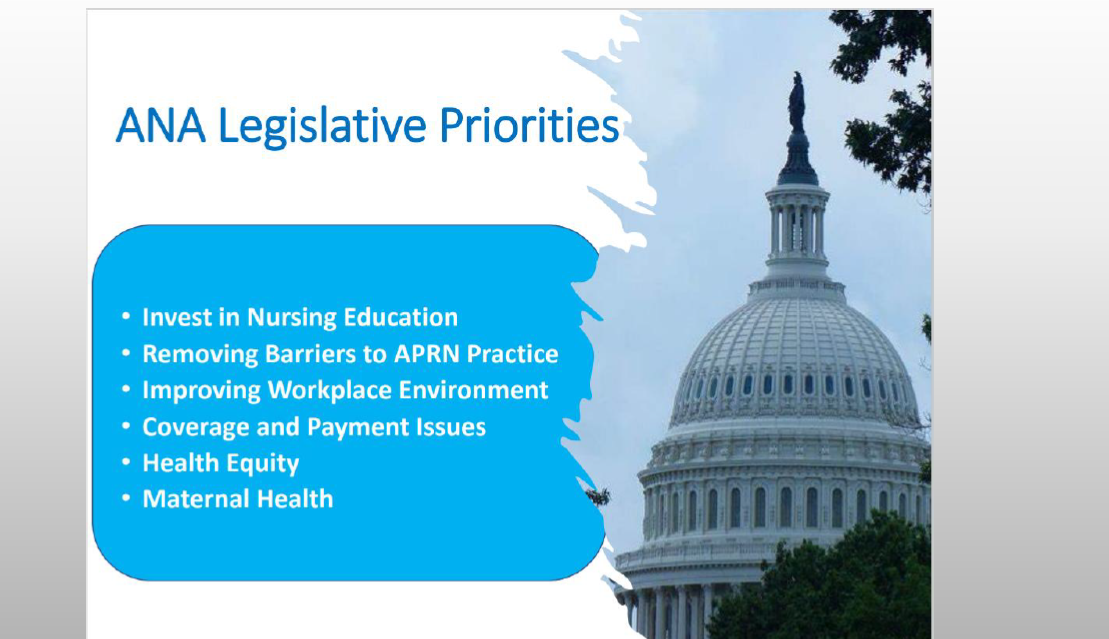
In Session 4, Michelle Buck, MS, APRN, CNS, senior policy advisor at
the National Council of State Boards of Nursing, and Zina Gontscharow,
MPP, senior policy advisor at ANA, examined how federal and state
advocacy and state nursing regulation and policy affect initiatives to
improve nurse staffing.
The final session, presented by ANA members Sherry Perkins, PhD, RN,
FAAN, president of Luminis Health Anne Arundel Medical Center, Matthew
McHugh, PhD, JD, MPH, RN, FAAN, professor and independence chair for
nursing education at University of Pennsylvania School of Nursing, and
Nancy Blake, PhD, RN, NEA-BC, FACHE, FAONL, FAAN, chief nursing officer
at Los Angeles General Medical Center, explored the evidence base for
establishing staffing standards. They also identified ways to advocate
for enforceable policies that support staffing standards and discussed
strategies for implementing them.
Collectively, these sessions offer nurses strategies and tools for
progress in achieving a sustainable nursing workforce.
American Nurse Journal. 2024; 19(4). Doi:
10.51256/ANJ042448
Reprinted with permission from ANA on the Frontline in American
Nurse Journal.