Nurses Service Organization (NSO), in collaboration with CNA, has published our 4th Edition of the NSO/CNA Nurse Liability Claim Report. It includes statistical data and case scenarios from CNA claim files, as well as risk management recommendations designed to help nurses reduce their malpractice exposures and improve patient safety.
You may access the complete report and additional Risk Control Spotlights at: www.nso.com/nurseclaimreport.
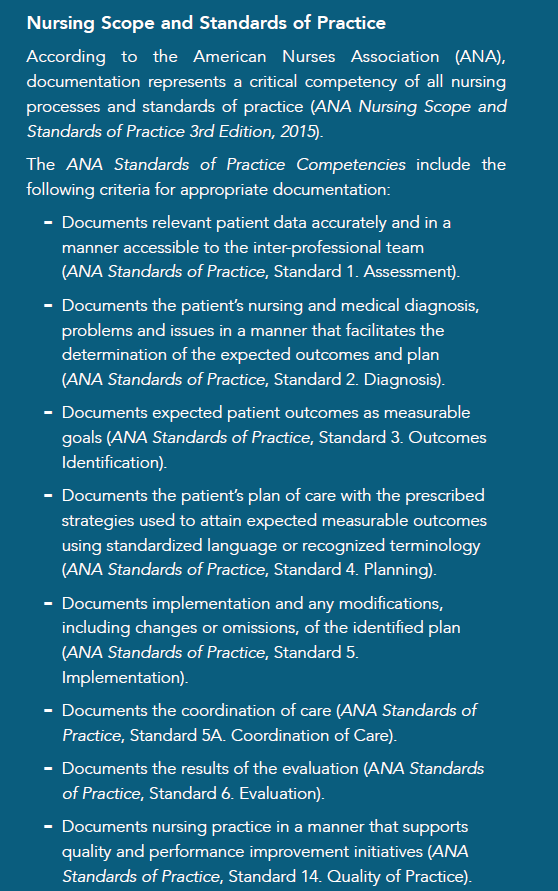
This Nurse Spotlight focuses on the analysis and risk recommendations regarding one of the most significant topics in the report and for nursing professionals: Healthcare Documentation.
Nursing Allegations Related to Healthcare Documentation
While documenting care represents a critical component of nursing processes and standards, the electronic health record [EHR] has posed a level of complexity for nurses who are often challenged with why, how, what and where to document in a patient’s EHR.
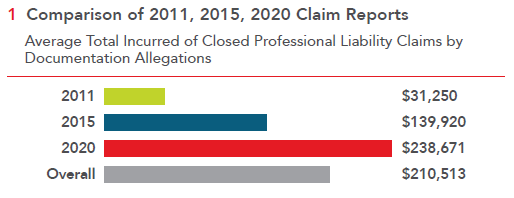
Documentation deficiencies are contributing factors to many nurse professional liability claims, as well as license protection matters. However, in the 4th Edition of the NSO/CNA Nurse Liability Claim Report, failure to document or falsifying documentation closed claims, as an allegation of professional liability, increased in distribution and severity when compared to the 2011 closed claim report and the 2015 closed claim report. Below is an example of a professional liability claim asserted against a nurse due to the failure to document:
Nurse Legal Case Study: Absence of documentation in violation of nursing standard of care
The patient was admitted to a rehabilitation facility after undergoing a right hip arthroplasty. Due to the patient’s other co-morbidities, her rehabilitation and recovery were slow and difficult. The patient’s health continued to deteriorate during her admission, until her death four months following admission. After the death of the patient, the family (plaintiffs) filed a complaint with the Department of Health (DOH) regarding the patient’s care at the facility.
The DOH investigated the complaint and cited 13 violations in the nursing standard of care. In particular, the DOH was critical of the absence of documentation related to care plans for the Foley catheter, the patient’s weight loss (from 93 to 77 pounds over four months), and neither shower nor self-care was documented for a timespan of more than five weeks. The insured registered nurse (RN) was the facility’s wound care nurse, and the DOH’s investigation found several violations of the nursing standard of care specific to the RN’s lack of documentation. First, the DON found a lack of documentation regarding a nursing incision wound for a period of approximately three weeks. The RN told the DOH surveyor that daily assessments were performed during that time, but since the wound care orders were to leave the right hip incision wound open to air, no treatment was performed, so the RN did not document anything. The patient also had a left heel pressure injury that was not healing, and the RN agreed that this non-healing injury had not been appropriately assessed or documented. Moreover, the director of nursing informed the DOH surveyor that the RN was required to perform weekly assessments on all patients in the facility. However, none were noted in the patient’s healthcare information records during a three-month period.
After seeing the DOH report, the family sued the facility and sued the insured RN separately. Knowing the challenges of the missing documentation and the negative DOH report, mediation was proposed with the plaintiffs. The total incurred amount to defend and settle this case on behalf of the insured RN was greater than $270,000.
In the 2011 closed claim report, 0.2 percent ($31,250) of all closed claims were related to inadequate or inappropriate documentation as the primary allegation. This data increased slightly to 0.5 percent ($139,920) in the 2015 closed claim report. Respectively, in the 2020 closed claim report, documentation allegations represent 2.0 percent ($238,761) of all closed claims.
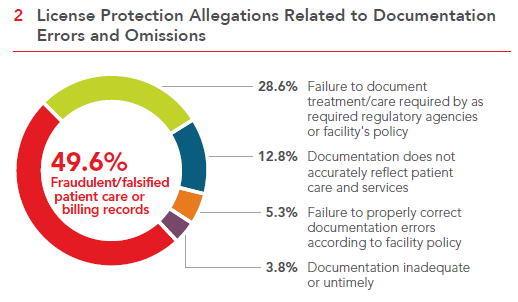
License Protection Allegations Related to Documentation Errors and Omissions
A license protection matter and a professional liability claim reflect a number of differences. First, a license protection matter only involves the cost of providing legal representation to defend the nurse before a regulatory agency or State Board of Nursing (SBON). On the other hand, professional liability claims include an indemnity or settlement payment. Second, license protection matters asserted against a nurse’s license to practice may or may not involve allegations related to patient treatment and care. The Nurse Spotlight: Defending Your License provides an overview of the role of the State Board of Nursing in the legal/regulatory system, describes the disciplinary process, and imparts helpful recommendations on defending yourself if you were to receive a complaint summons.
A nurse’s license is one’s livelihood, and its protection is paramount. A nurse’s practice and behavior is expected to be safe, competent, ethical, and in compliance with applicable laws and rules. However, when a complaint is filed, nurses must be equipped with the resources to adequately defend themselves. Being unprepared may represent the difference between a nurse retaining or losing the license to practice, a suspension, or fine.
The False Claims Act
While documentation deficiencies may result in a professional liability claim and/or a license protections matter, nurses also may be subject to federal and state sanctions for knowingly falsifying healthcare documentation under the federal False Claims Act (FCA). The FCA imposes liability on any person who submits a claim to the federal government that they know (or should have known) is false. An example may be a healthcare provider who submits a bill to Medicare for medical services they know they have not provided. The False Claims Act also imposes liability on an individual who may knowingly submit a false record in order to obtain payment from the government. For additional information on fraud and abuse laws, please see the Office of Inspector General’s provider education materials on Fraud & Abuse Laws.
Healthcare Documentation: Minimizing Risks, Maximizing Benefits
NSO/CNA is often asked about documentation risks and recommendations to minimize those risks. Nurses are certainly aware that there are patient healthcare documenting fundamentals. The healthcare information record is a legal document that is an essential tool to:
- Document the services provided regarding the patient’s illness or injury, response to treatment, and caregiver decisions;
- Communicate documented information about the patient’s plan of care and outcomes to the health care team
- Communicate information to other nursing professionals and healthcare providers;
- Support the appropriate information for billing coding; and
- Serve as the organization’s business and legal
Because complete, accurate and legible healthcare records constitute an essential risk management measure, nurses should maintain proper documentation practices and follow facility policies and procedures governing appropriate and comprehensive records documentation. The facility’s healthcare record documentation policies and procedures should address, at a minimum:
- Correcting documentation errors;
- Delineating appropriate use of the copy and paste function in the electronic healthcare record;
- Documenting practices during electronic system failures or outages (“down-time”);
- Maintaining patient confidentiality;
- Releasing patient healthcare information records and auditing practices; and
- Procedures for late or delayed
Risk Management Recommendations: Documentation
Maintaining a consistent, professional patient healthcare information record is integral to providing quality patient care, ensuring consistent communication among all professionals caring for the patient, documenting patient care outcomes and response and establishing the basis for an effective defense in the event of litigation. The following guidelines can help reduce risk:
Documentation – Clinical Content
-
Document nursing actions in accordance with facility requirements and patient needs, capturing the following information as clinically indicated:
- results of each nursing assessment
- pertinent nursing observations
- patient complaints or concerns
- significant changes in the patient’s condition
- any change in the patient’s care plan
- relevant monitoring findings, treatment or episode of care, as well as the patient’s response to that care
- facts relating to any patient accident or incident, including evidence of any injury, all parties notified, nursing care provided and patient’s condition after care is rendered
- laboratory and diagnostic test results, especially those that are abnormal and require provider notification and/or intervention
- referral and consultation requests and results
- telephone, face-to-face and electronic contacts with other members of the healthcare team, including the content of discussions and agreed-upon follow-up.
-
Document discussions with the patient about medical issues that require additional explanation by any healthcare practitioners and provider(s).
-
Record medications administered, including injections, ointments and infusions, as well as a description of the patient’s response as Also record self- administered medications.