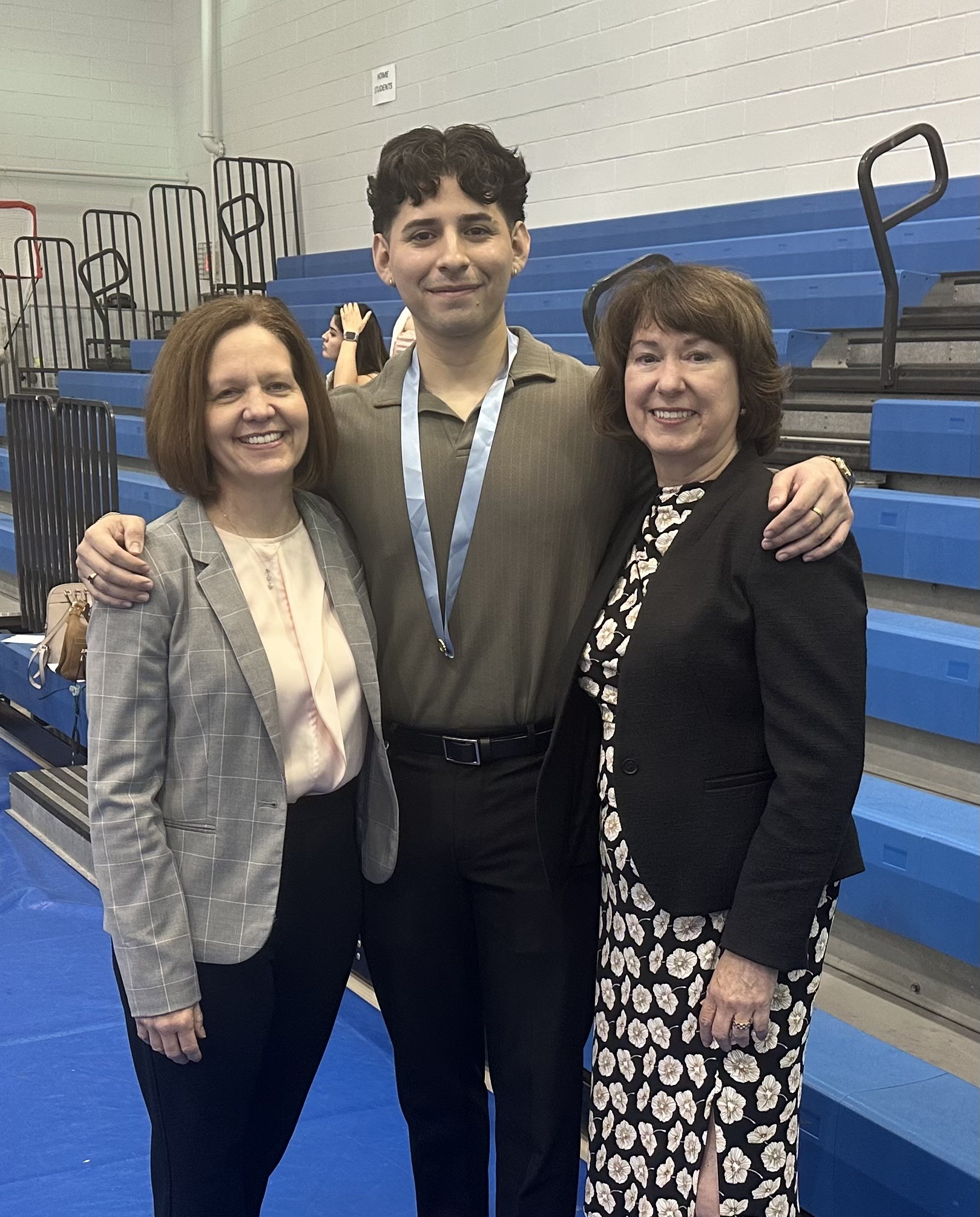
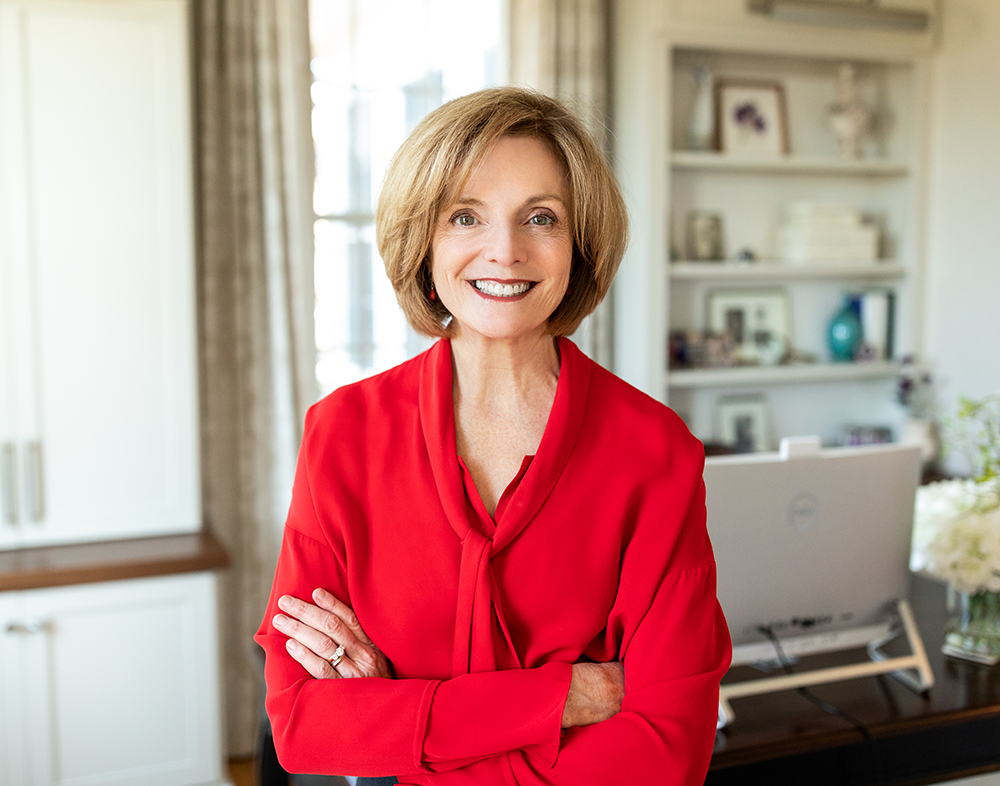
The Virginia Nurses Association and Foundation (VNA/VNF) are proud to welcome our new Chief Executive Officer, Lindsey Cardwell, MSN, RN, NPD-BC—a leader whose journey through clinical practice, professional development, and organizational service exemplifies the power of mentorship and the vital role nurses play as leaders across every care setting. As a registered nurse (RN) with nearly 20 years of experience, she brings deep passion and a bold vision for nursing in Virginia. Her story is a compelling reminder of why engaging with your professional association is not only valuable but essential, and how mentorship can shape a career and transform a profession. In this interview, she reflects on her journey, her leadership philosophy, and her hopes for the future of nursing in the commonwealth. Read on to learn more about Lindsey and her vision for VNA and VNF!
Tell us about your background and how it supports your new role as the CEO of the Virginia Nurses Association and Foundation.
I have been a registered nurse for almost two decades and am a proud graduate of the University of Virginia School of Nursing, where I earned both my BSN and MSN. My master’s degree focused on health systems management and leadership, which provided me the foundation to understand complex healthcare systems and lead change across organizations. That educational background has directly shaped my approach to leadership and prepared me to take on the role of CEO.
I began my career in a cardiovascular recovery unit, caring for patients immediately after open-heart surgery. During my fourth year of nursing school, I worked as a nurse extern on the same unit and received incredible mentorship from the nurses there. That experience solidified my decision to start my career in the cardiovascular recovery setting. As a new graduate, I was constantly challenged to learn and grow while working with a critical patient population. I was also fortunate to be surrounded by a team that helped shape me into not just a strong nurse, but a leader at the bedside.
My next step was transitioning into the realm of nursing professional development, a path I chose because I wanted to help drive change in nursing and healthcare through collaboration and education. I served as a Nursing Professional Development Specialist and later became the manager of our health system’s professional development department.
Nearly a decade into my career, the Virginia Nurses Association invited me to join the organization as its Director of Professional Development. In this role, I strengthened and expanded our American Nurses Credentialing Center (ANCC) Accredited Approval Unit, increasing access to continuing education for nurses across Virginia and beyond. I also led the effort to achieve ANCC Accredited Provider status, which allowed us to further develop offerings like our annual conferences, member webinars, and the Nurse Leadership Academy.
Throughout the last nine years, I have had the privilege of contributing to the mission-driven work of both VNA and VNF. I strongly believe in VNA’s mission to educate and advocate for registered nurses, and I am excited to continue growing the organization’s visibility and impact throughout the nursing and healthcare community.
What inspired you to become a nurse and how has that journey shaped your leadership style?
As a high school student, I attended the Central Virginia Governor’s School for Science and Technology. There, I had experiences that introduced me to the healthcare field such as assisting with breast cancer research, shadowing a physical therapist, and observing surgeries at my local hospital, to name a few. During my time in the operating room, an RN was serving as the lead for my experience and they left a lasting impression. I saw the nurse as a leader, a collaborator, and a powerful advocate for both patients and the healthcare team. This was the moment that initially sparked my desire to become a nurse.
These early experiences shaped how I see leadership in nursing. They taught me that nurses are not just caregivers, they are critical thinkers and drivers of progress. I believe it is essential to continue exposing students to nursing through STEM initiatives, career and technical education programs, and summer nursing camps so we can inspire the next generation of nurse leaders.
You've had a long and meaningful relationship with VNA as a student, a nurse, a board member, and as Director of Professional Development. What has kept you connected and committed?
Mentorship has been the cornerstone of my nursing journey, my leadership development, and my enduring connection to VNA. My very first clinical instructor at the University of Virginia encouraged me to attend the Virginia Nursing Students’ Association (VNSA) Annual Convention and to run for a board position. Due to her encouragement, I ran for and was elected VNSA President. She opened my eyes to the many ways nurses lead in clinical settings, communities, and professional organizations.
As VNSA President, I connected with the President of the VNA, who later encouraged me to run for Director-at-Large on the VNA Board. I initially questioned what I could offer as a new graduate, but she affirmed that my perspective was exactly what the board needed. That experience taught me the value of every voice in nursing, especially those just entering the profession.
Eventually, VNA created a board seat specifically for new graduate nurses, furthering our commitment to inclusion and mentorship. My own journey, from volunteer to staff, was fueled by the organization’s desire to expand professional development opportunities and support lifelong learning. These experiences have shown me the transformative power of mentorship and the importance of ensuring every nurse feels welcomed, supported, and empowered to lead.
With your deep understanding of the association and its community, what is your vision for its next chapter?
My vision is for the Virginia Nurses Association to serve as a convener, collaborator, and powerful advocate for nurses and the healthcare system. We must stay focused on our mission: to promote advocacy and education for registered nurses to advance practice and influence quality care delivery.
It is also critical that nurses across the commonwealth understand who we are, what we do, and why their membership matters. VNA is a membership organization for registered nurses. Our efforts are rooted in professional advocacy, with a strong focus on collaboration, education, and the convening of key stakeholders. Bringing people together is central to our mission. Through partnerships with schools of nursing, healthcare and community organizations, our board, chapter leaders, and our members, we unite diverse perspectives to advocate for the advancement of the nursing profession.
We want to raise the visibility of the VNA by listening to nurses, aligning our work with their evolving needs, and collaborating with our healthcare partners. Through that, we can build stronger solutions together.
You've been a passionate advocate for leadership development in nursing. Why is growing nurse leaders so essential right now?
As a volunteer with the VNF’s Virginia Action Coalition, I co-led a workgroup focused on advancing the call to action from the 2010 Institute of Medicine report, The Future of Nursing: Leading Change, Advancing Health, which emphasized that every nurse must be a leader, from the bedside to the boardroom.
Later, as VNA staff, I helped develop and launch the VNF’s Nurse Leadership Academy, which has already graduated more than 50 fellows. This work matters because nurses are on the front lines of care and their insight is essential in solving healthcare’s greatest challenges.
Leadership development gives nurses tools to enhance communication, navigate systems, and drive improvement. I am proud to continue advancing the Foundation’s mission: to improve community health by building a diverse, educated, and empowered nursing workforce through leadership development, research, and innovation.
How do you plan to stay connected with nurses across the state, from new graduates to seasoned professionals?
I am excited to work alongside our board, chapter leaders, and staff to expand our reach, deepen engagement, and strengthen connections with nurses at every stage of their careers. We are actively seeking opportunities to increase visibility and share the value of VNA, whether that is through presentations at nursing schools, conversations with healthcare organizations, or participation in community events.
We are also committed to developing new opportunities that foster collaboration and spark innovation among nurses across all practice environments. Creating space for shared learning and solution-building is essential to advancing our profession and supporting nurses in every role.
To ensure our work reflects the voices of our members, we will be connecting in multiple ways, including launching a member survey to gather feedback, ideas, and priorities. This input will be vital as we shape our future strategic plan and determine how we can best serve nurses across the commonwealth.
If your school, organization, or facility would like a VNA leader to speak about how nurses can engage with their professional association and drive meaningful impact, we encourage you to reach out to us!
Tell us more about your goals for partnering with nursing schools, employers, and communities to strengthen the profession.
This past year, we spent time listening to our members and engaging with leaders from nursing schools and healthcare organizations. One message came through clearly: there is a need for a shared space where we can collaboratively address workforce challenges.
We are working to create just that—a place for stakeholders to come together, learn from one another, and develop meaningful solutions. We look forward to sharing more details soon!
What would you say to a nurse who has never been involved with VNA before? Why should they join now?
I would start by asking, what are the biggest challenges you see facing nursing and healthcare, and what are you doing to help solve them? Then I would share this: Virginia is home to more than 140,000 RNs and advanced practice registered nurses (APRNs). Imagine the power of all those nurses coming together through one united voice.
The future of our profession, and of healthcare itself, is why every nurse should join VNA. And not just join but engage. Your voice matters!
What is something people may not know about your journey, professionally or personally, that influences how you lead?
Right before stepping into this role, I experienced healthcare from a different perspective—as a patient. That experience gave me profound insight into the vulnerability of being on the receiving end of care. You lose a sense of autonomy. You are facing something unfamiliar, often without understanding the rules or the roles.
I learned just how critical nurses are to the patient experience. When a nurse sees themselves as a leader, as a patient advocate and care coordinator, you feel safe. You feel heard. You know someone has your back.
I have spoken a lot about nurses as leaders, and I will continue to do so, because when nurses fully step into that role for their patients, their colleagues, and themselves, they truly make all the difference.
When you think about the legacy you would like to leave, what impact do you hope to have on VNA and the nurses we serve?
When I think about the legacy I hope to leave, it centers on helping every nurse see themselves as a leader, whether at the bedside, in the classroom, in administration, or at the policy table. I want to build a culture where nurses are confident in their voice, equipped with the tools to lead, and actively shaping the future of healthcare.
At the same time, I know that none of this work happens in isolation. I am deeply committed to collaborating with the VNA and VNF boards and our talented staff in every aspect of our work. Together, we will listen to our members, elevate their voices, and develop programs and advocacy efforts that reflect the evolving needs of nurses across the commonwealth.
Equally important is our ability to foster strong relationships outside of nursing with healthcare leaders, educators, policymakers, and community organizations because advancing the profession and improving patient outcomes requires shared vision and collective effort. I want VNA and VNF to be known not only as trusted voices in nursing, but also as respected partners across sectors.
Through mentorship, collaboration, innovation, and strategic partnerships, my hope is to strengthen the foundation of our organization and expand its reach. If I can help build a future where every nurse feels seen, heard, and supported, and where our association is leading boldly and collaboratively, I will consider that a legacy to be proud of.
Hear more from VNA and VNF's new CEO in the November edition of Virginia Nurses Today!