On July 1st, I officially began my two-year term as ANAMASS President. I am deeply honored and humbled by the opportunity to lead this valued organization and serve the dedicated nurses of Massachusetts.
Allow me to share a bit about my background and experience. I have been a Registered Nurse for over 30 years, a journey that has continually opened new doors and opportunities. I graduated with a BSN from Boston College on an Army ROTC scholarship and served in the Army Nurse Corps for five years at Walter Reed Army Medical Center in Washington, DC. Following my service, I worked as a Travel Nurse in Boston and DC, eventually settling at MGH and Tufts Medical Center. I earned a Master's in Nursing Administration from Northeastern University in 2005 and a Doctor of Philosophy from Endicott College in 2022. My career has included roles in Quality & Safety and Professional Development over the past 20 years. In 2022, I became the Nurse Director for Quality, Safety, & Professional Development at Newton-Wellesley Hospital, and my role has since expanded to Senior Director for Nursing Education, Quality, Research, and Innovation for the Mass General Brigham Community Hospital Division. I am board certified in Professional Development and as an Advanced Nurse Executive. None of this would have been possible without the unwavering support of my husband Pete and our two children, Megan and Jamie. I am also deeply grateful to the incredible mentors who have guided me along the way.
I joined ANAMASS in 2022 after attending the Spring Conference in Sutton, MA, where I presented my dissertation in a poster presentation. My research focused on health-promoting self-care practices among nurses and their perceived incidence of presenteeism. The health and wellbeing of nurses, and their ability to be authentically present and cognitively engaged in patient care, remain foundational to my professional practice. Inspired by the incredible ANAMASS team and the organization's offerings, I quickly became involved in the Professional Development Committee and the Board of Directors.
Over the past year as President-elect, I have attended the American Nurses Association (ANA) Leadership Summit, ANA Hill Day/Membership Assembly, and worked alongside Silda Melo, who transitioned from President to Immediate Past President. These experiences, combined with my background as an Army Nurse, Clinical Nurse, Nursing Professional Development Specialist, and Nurse Leader, have prepared me well for this role.
On behalf of ANAMASS, I would like to express deep gratitude to President Melo for her contributions to advancing nursing in Massachusetts. President Melo began her involvement in ANAMASS as a newly graduated RN Director, one of two New Grad positions on the Board of Directors, and advanced to the role of President. During her tenure, she lobbied, advocated, and testified for numerous issues critical to our nursing workforce across the Commonwealth. Through her dedicated leadership and years of advocacy, Massachusetts became one of 43 states in the US to approve the Nurse Licensure Compact (NLC). When Governor Healey signed the legislation adopting the NLC in November 2024, it enhances nurses' mobility to practice across state lines, increases access to care, and improves patient protection through standardized licensing requirements. I applaud President Melo for her hard work in achieving this monumental accomplishment.
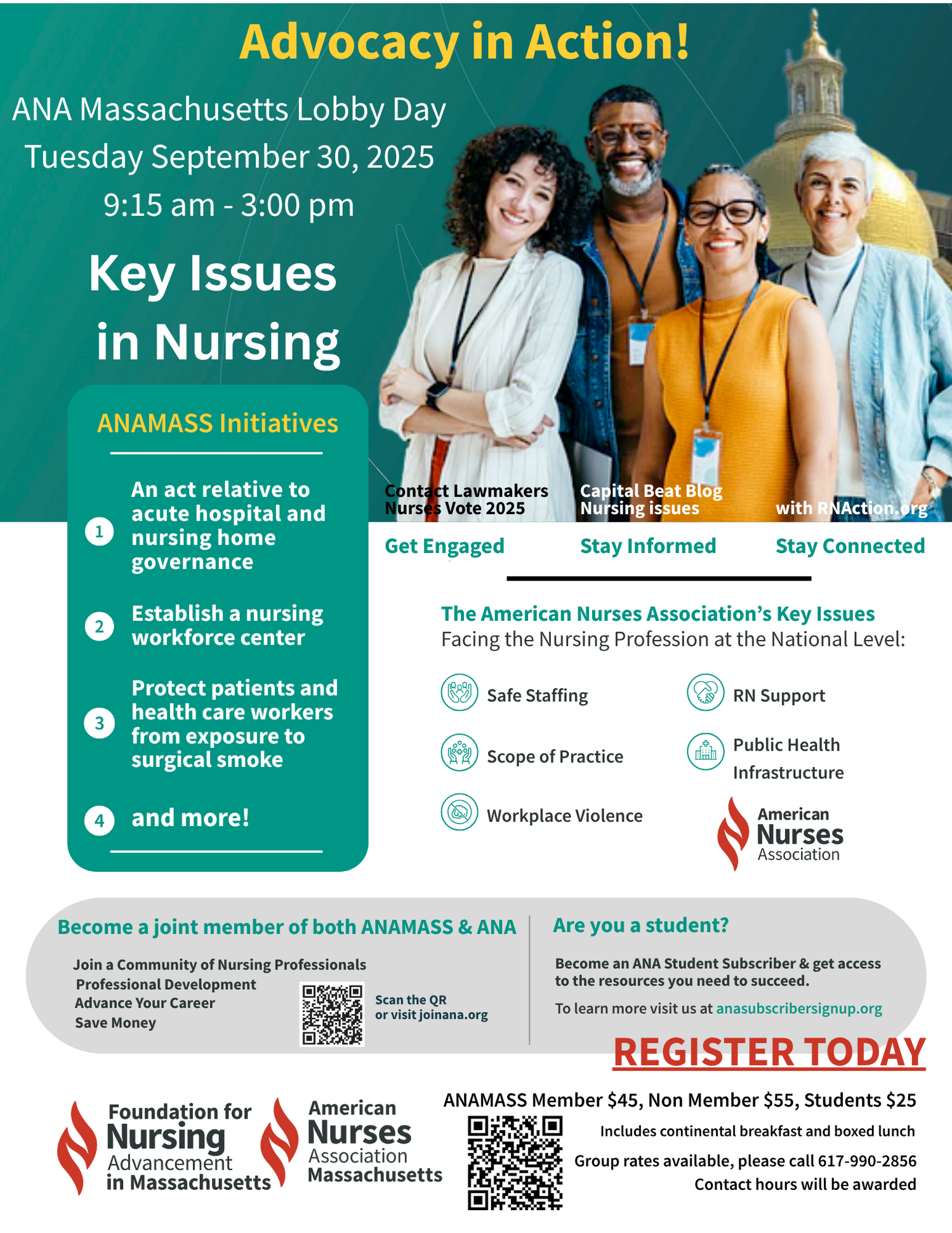
The nursing profession is facing challenging times, with many legislative challenges ahead. ANAMASS Health Policy Committee Members and Membership Assembly participants spent a full day on Capitol Hill meeting with Massachusetts legislators and their aides, lobbying and advocating to ensure they fully understood the impacts of the proposed Medicaid reforms outlined in the Big Beautiful Bill. Despite leaving over 450 stethoscopes as reminders, the Senate and House of Representatives passed the bill, which was signed into law on July 4th. As a result, reduced Medicaid funding will undoubtedly impact healthcare jobs, wages, and uncompensated care, while potentially increasing nursing workloads by caring for patients with higher acuity. Currently, Medicaid funding supports the demand for nurses, sustains jobs in home care, long-term care, and community settings, and provides payment for safety net hospitals where many Massachusetts nurses are employed. This is where the power of nurses, the power of our voices and our advocacy---to do what we know is best for patients, families, and communities---becomes critically important.
The journey ahead is uncertain, but together, nurses have the power to drive change, advocate for those we serve, and be transformative. I look forward to advancing nursing practice across our Commonwealth and am grateful for the opportunity to work alongside all nurses in Massachusetts.