Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Harvard university press.
Centers for Disease Control and Prevention. (2024a, December 20). Childhood Obesity Facts. Obesity. https://www.cdc.gov/obesity/childhood-obesity-facts/childhood-obesity-facts.html
Centers for Disease Control and Prevention. (2024b, December 20). Preventing Childhood Obesity: 6 Things Families Can Do. Obesity. https://www.cdc.gov/obesity/family-action/index.html
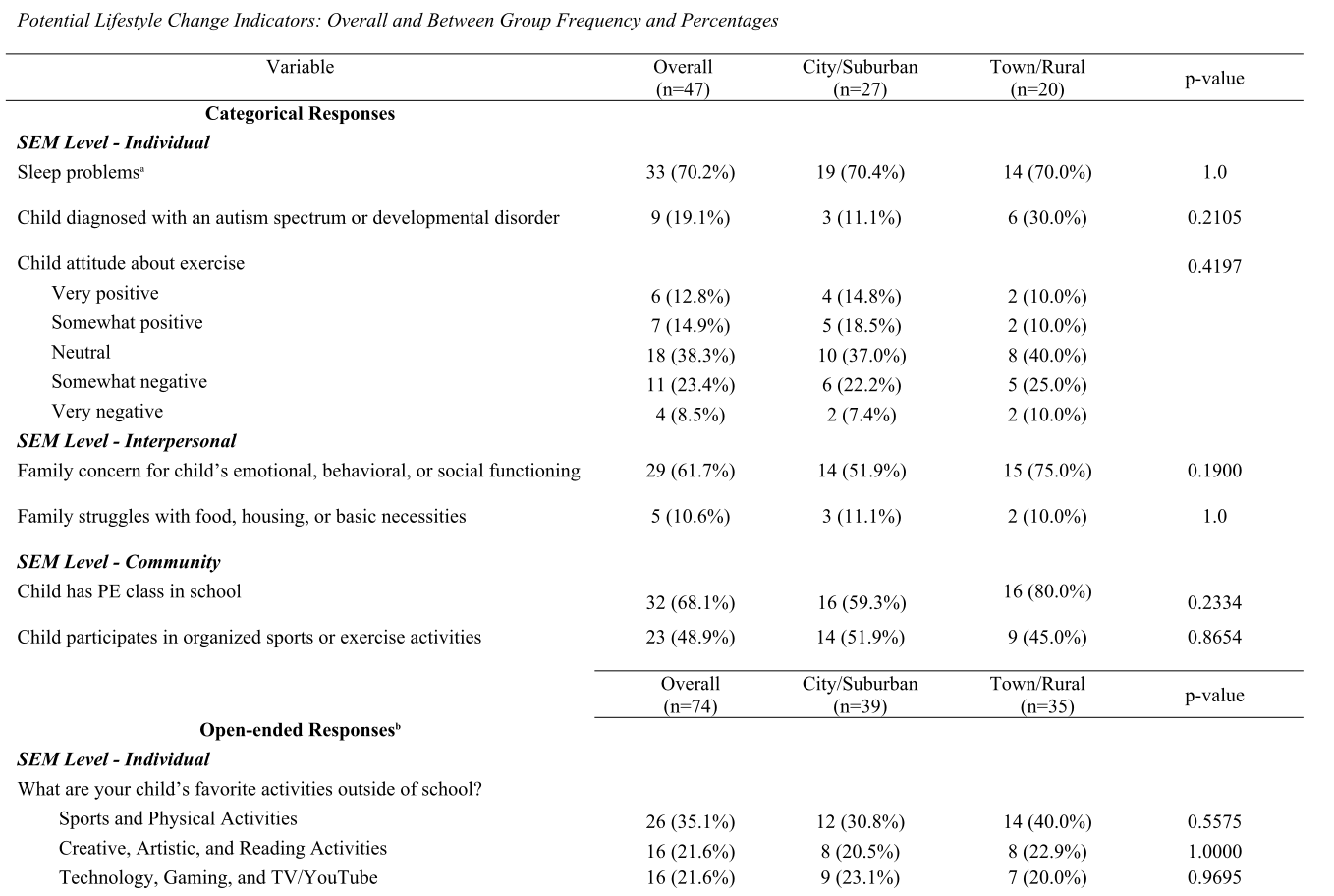
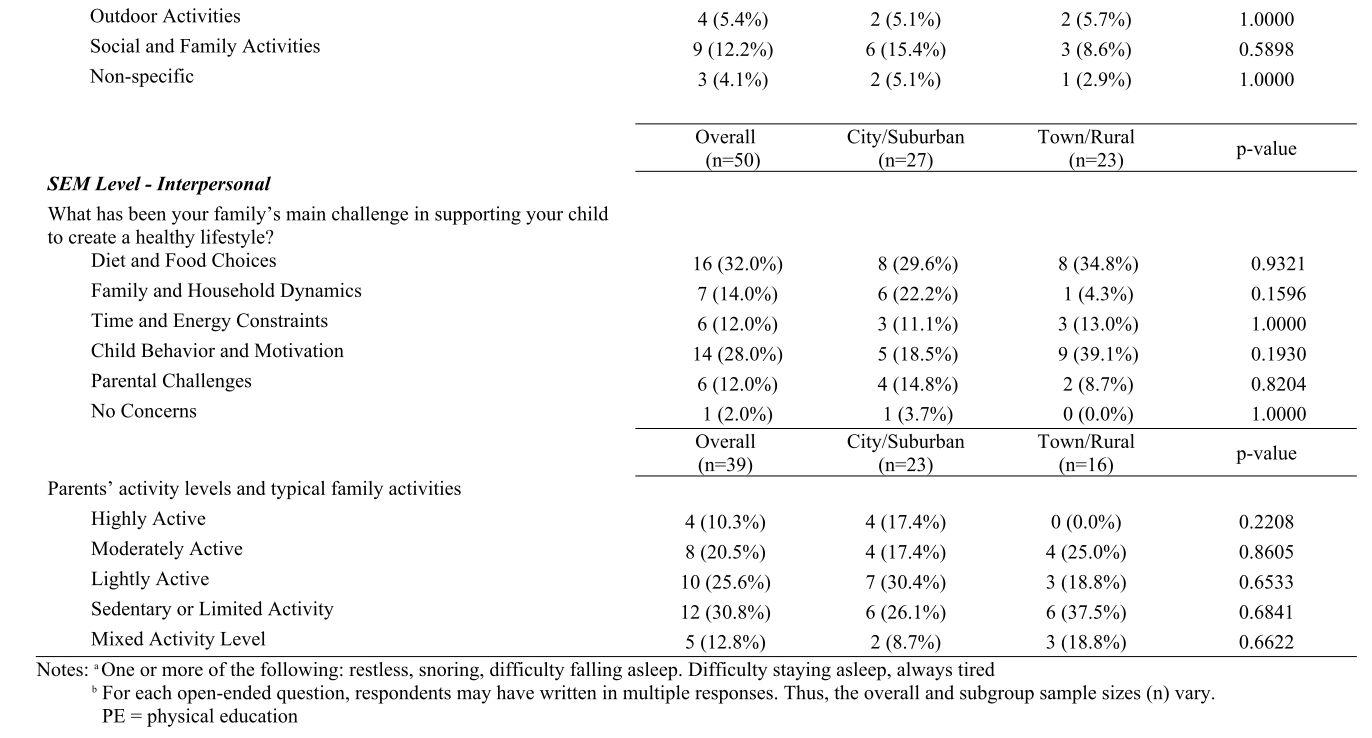
Crouch, E., Abshire, D. A., Wirth, M. D., Hung, P., & Benavidez, G. A. (2023). Rural-urban differences in overweight and obesity, physical activity, and food security among children and adolescents. Preventing Chronic Disease, 20, E92. https://doi.org/10.5888/pcd20.230136
Fulkerson, J. A., Horning, M. L., Barr-Anderson, D. J., Linde, J. A., Sidebottom, A. C., Lindberg, R., Friend, S., Flattum, C., & Freese, R. L. (2021). Universal childhood obesity prevention in a rural community: Study design, methods and baseline participant characteristics of the NU-HOME randomized controlled trial. Contemporary Clinical Trials, 100, 106160. https://doi.org/10.1016/j.cct.2020.106160
Healthy People 2030. (n.d.). Social Determinants of Health. Health.Gov. Retrieved July 23, 2024, from https://health.gov/healthypeople/priority-areas/social-determinants-health#:~:text=Social%20determinants%20of%20health%20(SDOH,Economic%20Stability
Idaho Administrative Code: Rules Governing Thoroughness, No. IDAPA 08.02.03. https://adminrules.idaho.gov/rules/current/08/080203.pdf
Idaho Department of Health and Welfare. (n.d.). Rural Health and Underserved Areas. Retrieved February 14, 2025, from https://healthandwelfare.idaho.gov/providers/rural-health-and-underserved-areas/rural-health-and-underserved-areas
Kelleher, E., Davoren, M. P., Harrington, J. M., Shiely, F., Perry, I. J., & McHugh, S. M. (2017). Barriers and facilitators to initial and continued attendance at community-based lifestyle programmes among families of overweight and obese children: A systematic review. Obesity Reviews: An Official Journal of the International Association for the Study of Obesity, 18(2), 183--194. https://doi.org/10.1111/obr.12478
L'Hôte, E., Levay, K., & Nicky, H. (2021). Changing the childhood obesity conversation to improve children's health. Washington DC: FrameWorks Institute. https://frameworksuk.org/resources/changing-the-childhood-obesity-conversation-to-improve-childrens-health/
Lim, C. S., & Janicke, D. M. (2013). Barriers related to delivering pediatric weight management interventions to children and families from rural communities. Children's Health Care, 42(3), 214--230. https://doi.org/10.1080/02739615.2013.816596
Liu, R., Figueroa, R., Brink, H. V., Vorland, C. J., Auckburally, S., Johnson, L., Garay, J., Brown, T., Simon, S., & Ells, L. (2024). The efficacy of sleep lifestyle interventions for the management of overweight or obesity in children: a systematic review and meta-analysis. BMC Public Health, 24(1), 321. https://doi.org/10.1186/s12889-024-17708-6
Lundh, H., Arvidsson, D., Greven, C., Fridolfsson, J., Börjesson, M., Boman, C., Lauruschkus, K., Lundqvist, S., Melin, K., & Bernhardsson, S. (2025). Physical activity and sedentary behaviour amongst children with obesity---Exploring cross-sectional associations between child and parent. Journal of Activity, Sedentary and Sleep Behaviors, 4(1), 2. https://doi.org/10.1186/s44167-025-00072-0
Moeller, N. C., Oestergaard, L., Rasmussen, M. G. B., Schmidt-Persson, J., Larsen, K. T., & Juhl, C. B. (2024). How to get children moving? The effectiveness of school-based interventions promoting physical activity in children and adolescents - A systematic review and meta-analysis of randomized controlled- and controlled studies. Health & Place, 89, 103333. https://doi.org/10.1016/j.healthplace.2024.103333
Ogden, C. L., Fryar, C. D., Hales, C. M., Carroll, M. D., Aoki, Y., & Freedman, D. S. (2018). Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013-2016. JAMA, 319(23), 2410--2418. https://doi.org/10.1001/jama.2018.5158
Ohri-Vachaspati, P., DeLia, D., DeWeese, R. S., Crespo, N. C., Todd, M., & Yedidia, M. J. (2015). The relative contribution of layers of the Social Ecological Model to childhood obesity. Public Health Nutrition, 18(11), 2055--2066. doi:10.1017/S1368980014002365
Pereira, M. M. C. E., Padez, C. M. P., & Nogueira, H. G. D. S. M. (2019). Describing studies on childhood obesity determinants by Socio-Ecological Model level: A scoping review to identify gaps and provide guidance for future research. International Journal of Obesity (2005), 43(10), 1883--1890. https://doi.org/10.1038/s41366-019-0411-3
Potter, W. J., & Levine‐Donnerstein, D. (1999). Rethinking validity and reliability in content analysis. Journal of Applied Communication Research, 27(3), 258--284. https://doi.org/10.1080/00909889909365539
Sammels, O., Karjalainen, L., Dahlgren, J., & Wentz, E. (2022). Autism Spectrum Disorder and Obesity in Children: A Systematic Review and Meta-Analysis. Obesity Facts, 15(3), 305--320. https://doi.org/10.1159/000523943
Strochlic, R., Au, L., & Ritchie, L. (2017). Is urban--rural location associated with weight status in school children? An examination of 42 small and rural Californian counties. Rural and Remote Health, 17(2). https://doi.org/10.22605/RRH3966
U.S. Department of Education. (n.d.). Common Core of Data (CCD). National Center for Education Statistics. Retrieved January 30, 2025, from https://nces.ed.gov/ccd/
U.S. Health Resources and Services Administration. (n.d.). What Is Shortage Designation? Bureau of Health Workforce. Retrieved January 30, 2025, from https://bhw.hrsa.gov/workforce-shortage-areas/shortage-designation#mups
Williams, A. S., Ge, B., Petroski, G., Kruse, R. L., McElroy, J. A., & Koopman, R. J. (2018). Socioeconomic Status and Other Factors Associated with Childhood Obesity. Journal of the American Board of Family Medicine : JABFM, 31(4), 514--521. https://doi.org/10.3122/jabfm.2018.04.170261