As nurses, we know that health is not simply the absence of illness; it's the presence of equity, opportunity, and hope. Every day, nurses lead with compassion, courage, and commitment to the well-being of our patients and communities. The Virginia Nurses Foundation (VNF) exists to sustain and amplify that mission, ensuring that every nurse has the resources and opportunities to make a lasting difference.
Philanthropy is the lifeblood that nourishes the roots of positive change. When you donate to VNF, you become an architect of a healthier, more equitable Virginia, one where the nursing profession continues to thrive and every community has access to compassionate, high-quality care.
Choose Your Area of Impact
Whether your heart leads you to advance equity, policy, leadership, or mental health, your contribution directly supports initiatives that transform lives and strengthen our profession.
Dr. Vivienne McDaniel Health Equity Scholarship (Donate Here)
This scholarship honors Dr. Vivienne McDaniel, a visionary leader whose legacy continues to shape the nursing landscape through her commitment to diversity, equity, and inclusion. As the inaugural Chair of the VNA & VNF DEI Council and a past Diversity Ambassador for VNF, Dr. McDaniel championed ethical, inclusive care and inspired countless nurses to do the same. Your donation helps us continue that vital work, supporting nurses who are driving health equity forward across the commonwealth.
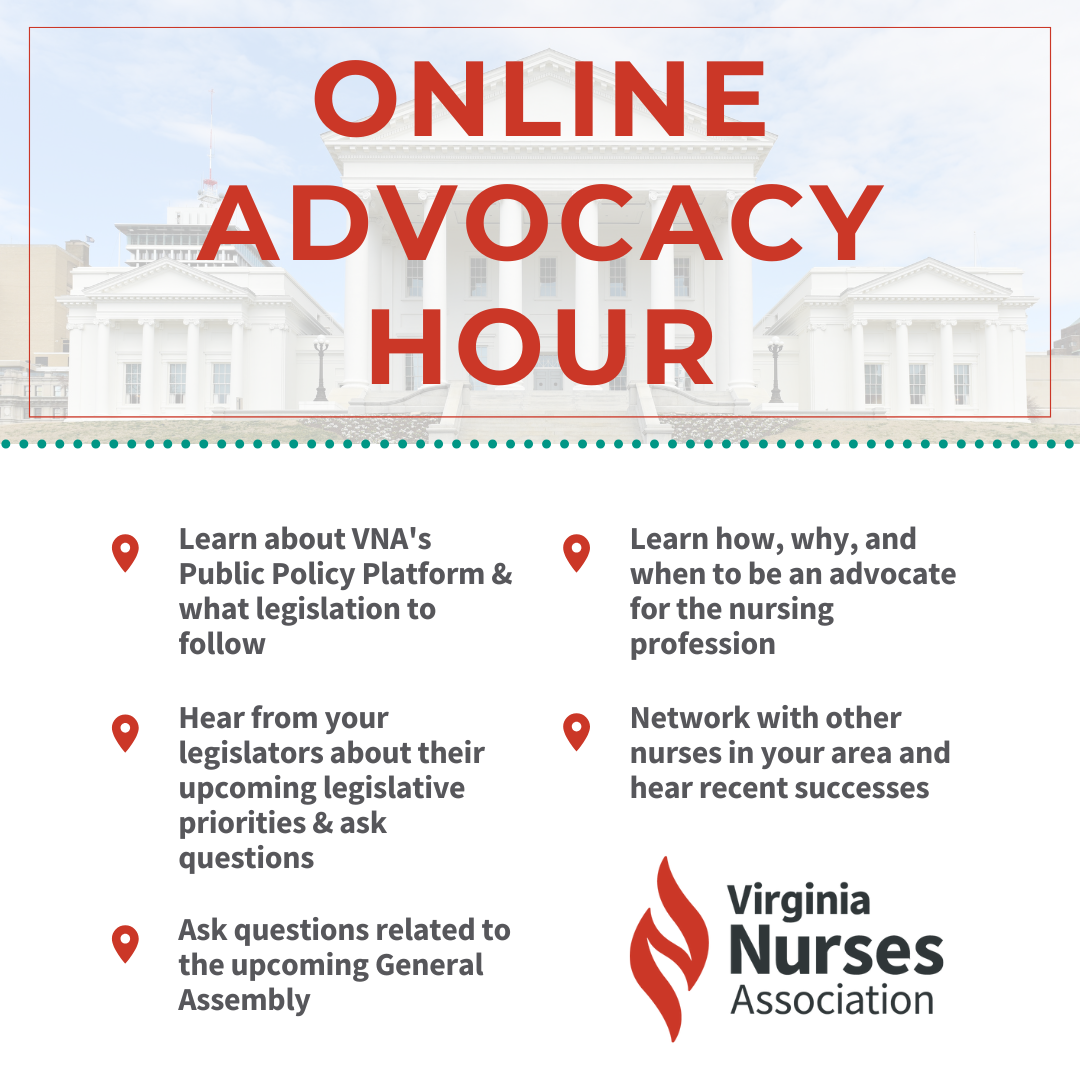
Leslie Herdegen Public Policy Scholarship (Donate Here)
Established to honor Leslie Herdegen Rohrer, a passionate advocate who spent two decades advancing causes that improved mental health, nursing practice, and community well-being across Virginia. This scholarship empowers nurses to develop as public policy leaders, equipping them with the knowledge and influence to shape the future of healthcare legislation.
Nightingale Legacy Fund & Nurse Leadership Development (Donate Here)
Leadership is the light that guides our profession. The Nightingale Legacy Fund supports the Nurse Leadership Academy and allows you to honor a nurse leader who has inspired you. Every contribution not only strengthens leadership development but also sends a message of gratitude, and your honoree will be notified of your recognition.
Lauren Goodloe Nursing Scholarship (Donate Here)
Created to honor Dr. Lauren Goodloe, a beloved leader and educator whose career embodied excellence, education, and service. By contributing, you invest in the growth of emerging nurse leaders who will carry forward her spirit of strength and advocacy.
Mental Health, DEI, and More (Donate Here)
From addressing mental health distress to advancing diversity and inclusion, VNF is committed to building healthier communities. One in 14 Virginians faces mental health challenges, often intertwined with social determinants of health. Your support helps nurses respond to these challenges with compassion, evidence-based care, and advocacy for systemic change.
As professional nurses, we also hold a shared responsibility to confront racism, injustice, and inequity. VNF's Diversity, Equity & Inclusion Council continues to tackle these challenges head-on, creating spaces where every nurse and every patient feels seen and valued.
Nurses Change Lives License Plate (Order Here)
Drive with pride! The VNF "Nurses Change Lives" license plate celebrates the vital work of nurses across Virginia. With each purchase, $15 supports VNF scholarships and nursing education initiatives. A perfect gift for pinning ceremonies, promotions, and retirement, share the gift of nursing pride that keeps on giving.
Join Us on Giving Tuesday -- December 2, 2025 (Learn More)
Giving Tuesday reminds us that generosity, whether through time, talent, or treasure, has the power to change the world. On this Global Day of Giving, we invite you to support the Virginia Nurses Foundation and help us continue building a future rooted in compassion, equity, and leadership.
Every act of generosity counts. Every dollar makes a difference. Together, we are cultivating health, advancing equity, and shaping the future of nursing in Virginia.