As a nursing leader, I attribute much of my success to my involvement with professional organizations like ANA, ANCC, and AONL. These organizations have been instrumental in my professional development, and I strongly encourage all nurses to join and participate in their specialty-focused organizations.
Benefits of Membership
- Professional Development: Access to continuing education, certification programs, and specialization opportunities.
- Networking Opportunities: Build relationships, share best practices, and collaborate with peers and industry leaders.
- Advocacy and Influence: Participate in policy decisions, advocacy efforts, and representation at local, state, and national levels.
- Access to Resources: Stay updated with publications, research, career resources, and job boards.
- Professional Recognition and Credibility: Demonstrate commitment to the profession, enhance credibility, and receive recognition for expertise.
- Leadership Development: Develop leadership skills, access mentorship opportunities, and prepare for higher levels of responsibility.
- Sense of Community and Belonging: Foster a sense of belonging, support, and solidarity with fellow nurses.
- Impact on Quality of Care: Contribute to standard setting, innovation in practice, and improved patient outcomes.
- Personal Fulfillment: Find purpose, empowerment, and fulfillment in advancing the nursing profession and improving patient care.
Conclusion
Membership in nursing professional organizations is crucial for your personal growth, professional development, advocacy, and improving patient care. Join, participate, and find your voice in your specialty-focused organization. You won't regret it.
Here is a summary of this year’s AONL Conference in New Orleans
The AONL 2024 conference focused on empowering frontline nursing leaders, fostering collaboration across the healthcare continuum, and advancing healthcare standards.
Keynote speakers included:
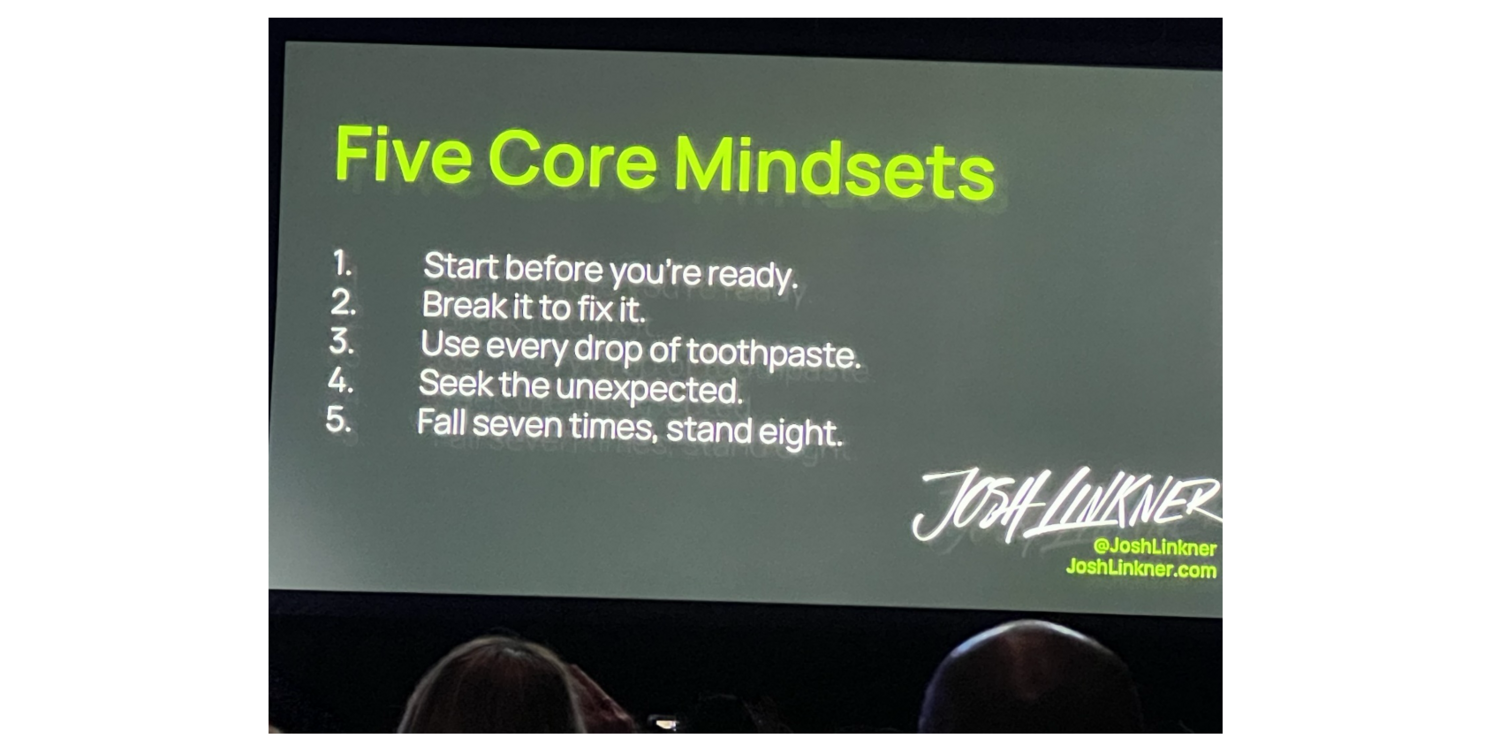
- Josh Linkner—a New York Timesbestselling author—is a rare blend of business, art, and science. He passionately believes that all human beings have incredible creative capacity, and he’s on a mission to unlock inventive thinking and creative problem solving to help leaders, individuals, and communities soar. Josh has been the founder and CEO of 5 tech companies and is the author of 4 books including the New York Times bestsellers, Disciplined Dreaming and The Road to Reinvention.
- Keller Rinaudois chief executive officer and cofounder of Zipline, which delivers life-saving medical supplies to hospitals and health centers via autonomous drones built in its San Francisco Bay area headquarters. Zipline started operations in Rwanda in 2016 and now has delivery services in 5 African counties, Japan, and the United States.
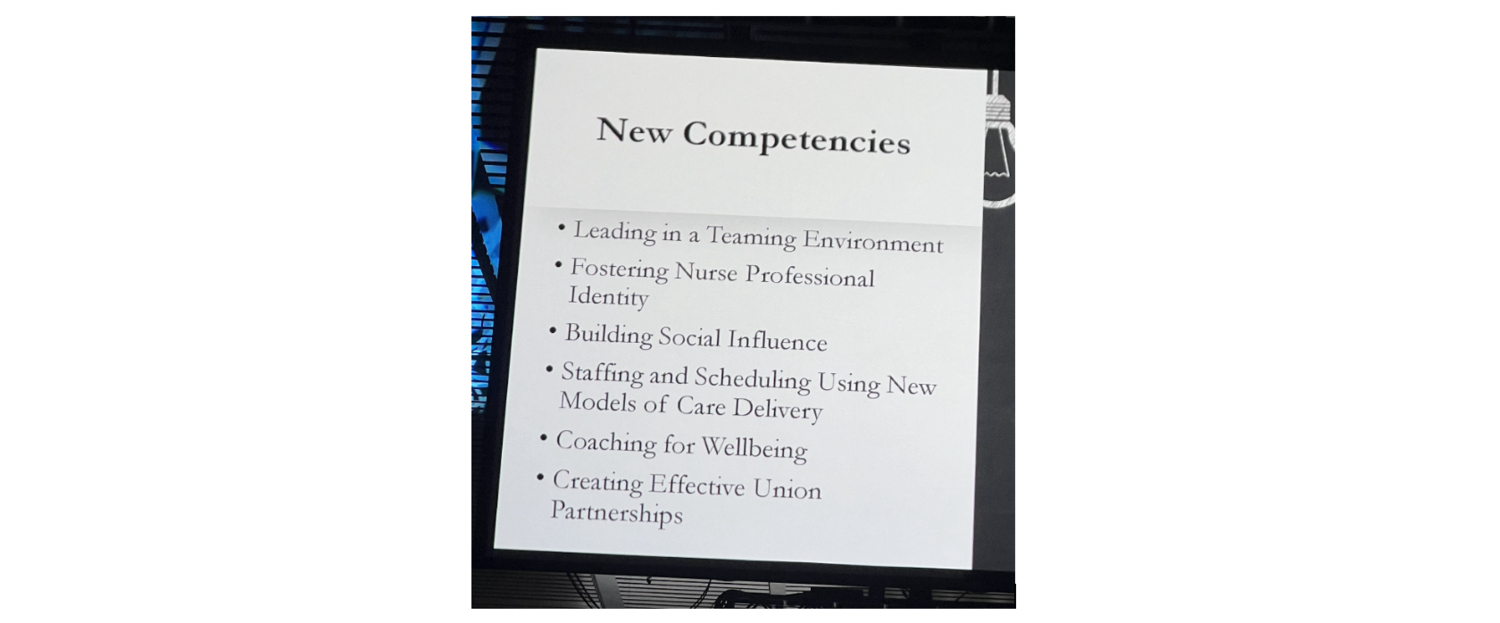
- Rose Sherman, EdD, RN, NEA-BC, FAAN, is nationally known for her work in helping current and future nurse leaders develop their leadership skills. Sherman is an emeritus professor at the Christine E. Lynn College of Nursing at Florida Atlantic University, Boca Raton, and currently serves as a faculty member in the Marian K. Shaughnessy Nursing Leadership Academy at Case Western Reserve University, Cleveland, Ohio.
- Amy Walter, whohas built a reputation as an accurate, objective, and insightful political analyst with unparalleled access to campaign insiders and decision-makers. Walter is the publisher and editor-in-chief of the Cook Political Report with Amy Walter and a frequent on-air analyst.
Key takeaways include:
- Empowering Frontline Managers: Supporting and developing frontline managers is crucial for shaping organizational culture and driving positive outcomes.
- Fostering Collaboration: Interdisciplinary partnerships and cross-sector collaborations can drive innovation and improve patient outcomes.
- Continuous Improvement: Elevating healthcare standards and driving positive change requires a shared commitment to excellence and innovation.