Introduction
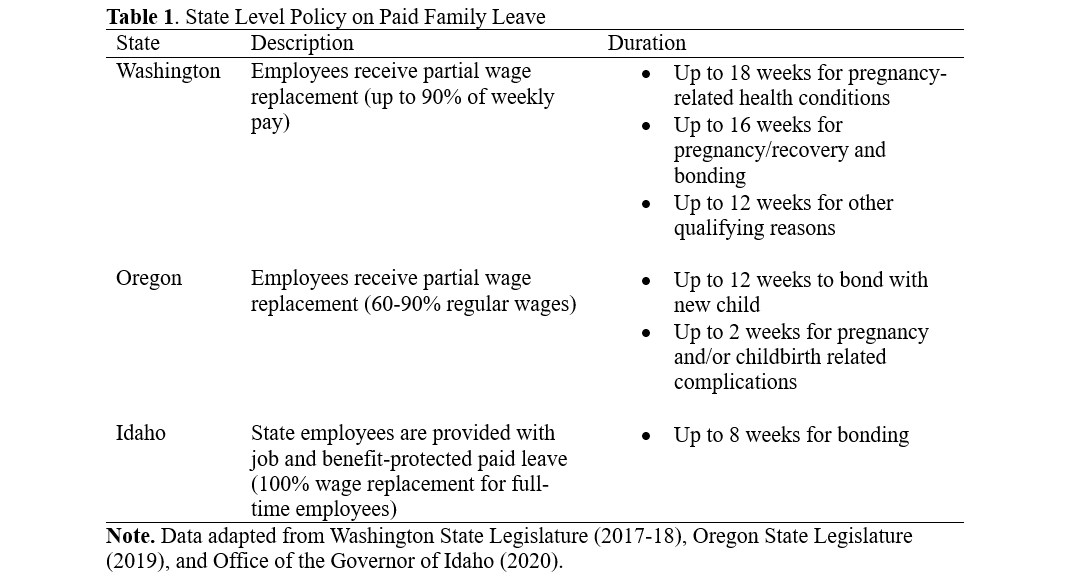
Between 2022 and 2024, Idaho agencies that employ nurses continued to experience staffing shortages. Since 2016, the Idaho Center for Nursing has supported strategies to increase the number of nurses working in Idaho, to improve their educational levels, to ease credit transferability between schools, to improve their work environments, and to support public policy that positively impacted nurses. On a biennial basis these factors have been evaluated since 2000, and the findings reported publicly.
Nursing workforce reporting was historically a national activity whereby researchers from the Department of Labor looked at the number of licensed nurses and their geographic distribution and arrived at a total number of nurses in the United States. There were issues with this methodology because it could not account for individual nurses who were licensed in more than one state, and thus there was a duplicate count that some researchers reported was as high as 500,000 nurses. Today, the National Council of State Boards of Nursing (NCSBN) reports that there are 5,744,766 RN licenses issued in the U.S., but there are only 4,845,706 RNs (NCSBN, 2024). Thus, the duplicate RN license count is now nearly 900,000.
To help alleviate the problems associated with evaluating the nursing workforce, the Robert Wood Johnson Foundation funded a national effort in 2000 aimed to establish a nursing workforce center in each state. The outcome was the establishment of the National Forum of State Workforce Centers (NFSNWC) that works with each state's individual workforce center and that established the Nursing Workforce Minimum Data Sets (NFSNWC, 2004).
In Idaho, the initial grant was managed by Boise State University. After RWJF funding stopped in 2006 it moved to the Idaho Board of Nursing (BON). Because the BON only had access to supply and education data and there were issues associated with job demand data analysis, the BON contracted with the Idaho Department of Labor for data reporting and analysis 2011-2015. The report was transferred to the Idaho Center for Nursing (ICN) in 2016 for comprehensive data assimilation and evaluation. Today the ICN is the umbrella nursing organization that supports the Idaho Nursing Workforce Center.
The ICN's workforce center has been funded by the BON's designated fund balance and supports the research, analysis and dissemination of the report's data. The report uses three nationally vetted data sets so that it is possible to compare state to state information using the same data collection tools and analysis framework. They are supply, education and job demand data. An additional nurse self-reported survey is also offered in Idaho.
States that have in excess of 100,000 licensed nurses use a sample survey. In Idaho, because we have less than 20,000 resident nurses, we can complete a population survey whereby the data from each individual nurse is analyzed and reported. To maintain confidentiality of the individual nurse, all data is reported as aggregate and cannot be linked to individual nurses.
Supply data is based on the June 25, 2024, nurse license database information that was available on the National Council of State Boards of Nursing (NCSBN) Optimal Regulatory Board System (ORBS) report that was accessed by Idaho Board of Nursing staff. Additional information from the newly developed Idaho Department of Professional Licensing OASIS system that was implemented in July 2024 was also used.
Licensed Practical Nurse supply data shows that there are 3,467 LPNs with active licenses and 3,105 are Idaho residents. The other 392 reside in other states or are in the military. This is 72 fewer LPNs than in 2022. Of the 3,105 Idaho LPNs, 283 report that they are not employed and not seeking work. The age of these nurses is an important consideration, with 242 (7.8%) being over the retirement age of 67 years. Only 1,067 (34%) are younger than 40 years.
Registered Nurse supply data shows that there are 22,845 RNs with active licenses and 2,487 of them are APRNs. Because APRNs do not commonly fill RN roles, removing them from the RN count yields 20,358 for the potential RN workforce. This is a 1,708 RN increase from 2022. However, 1,399 (7%) of RNs are older than the retirement age of 67 years, and 46 are older than 80 years. Considering age, an adjusted RN workforce count can be made at 18,959 nurses, which is 309 more working RNs than in 2022.
Geographic distribution is significant. The 2022 workforce report identified a geographic shift from small towns and rural communities to either one large town in a region or to the Boise area. In 2024 there is evidence that this movement has slowed and rural Idaho actually gained 520 more nurses than were rural in 2022. Some of this could be the result of the Idaho Rural Nurse Loan Repayment program that went into effect in 2023. Still, the greatest number of RNs live in the Boise area at 9,071 (44.5%).
An important factor in evaluating nurse employment potential in Idaho is that 90% of all nurses, both RN and LPN, are already employed either full or part time. This is compared to an average of 63% being employed in all other professions. Thus, the pool of nurses who are available to hire is very limited.
Advanced Practice Registered Nurses (APRNs) are divided into the 4 job categories of nurse practitioner, nurse anesthetist, nurse midwife and clinical nurse specialist. There is a significant number of each category who are licensed in Idaho but who do not live in Idaho.
Of 3,730 NPs, only 1,636 are Idaho residents. This is 71 fewer NPs working in Idaho in 2024 than in 2022. Half of the NPs live in the Boise area. Only 42 NPs reported that they practice in communities that do not have providers other than NPs, and 72% work for healthcare systems or physicians. The remainder are educators, government employees or in private practice.
There are 724 licensed CRNAs, representing 493 who live in Idaho. Of this, 201 live in the Boise area with 292 in other Idaho communities and 231 in other states. This is an increase of 43 CRNAs in Idaho.
Nurse Midwives have 97 total licensed, with 76 as Idaho residents. They are primarily in Boise, Nampa, Idaho Falls, and Coeur d'Alene.
Clinical Nurse Specialist have 49 licensed with 30 as Idaho residents, and 20 of those are in Boise. This is an overall decrease by 9 CNSs since 2022.
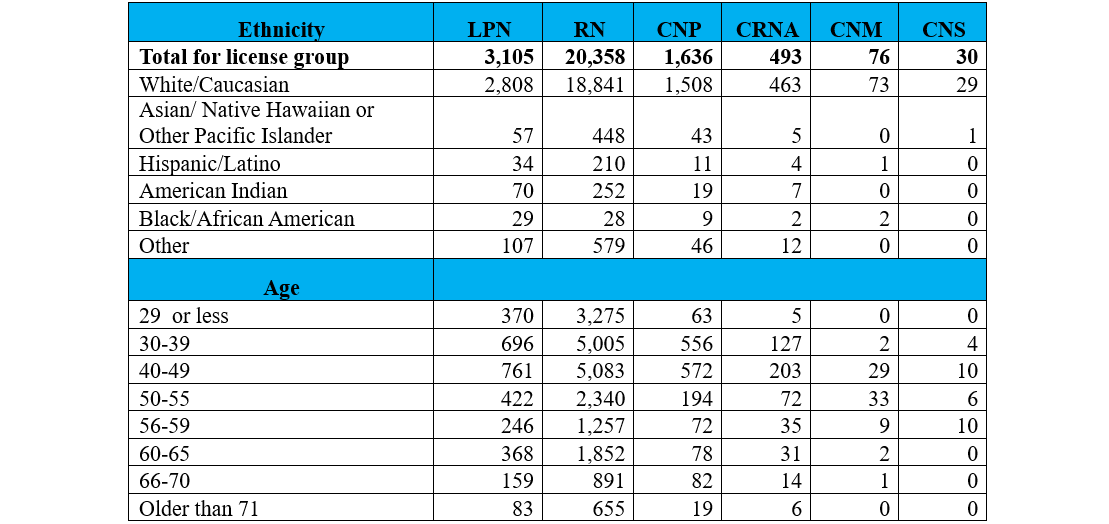
Ethnicity and age data is presented and is consistent with previous reports.
2024 Nurse demographic data for Idaho residents
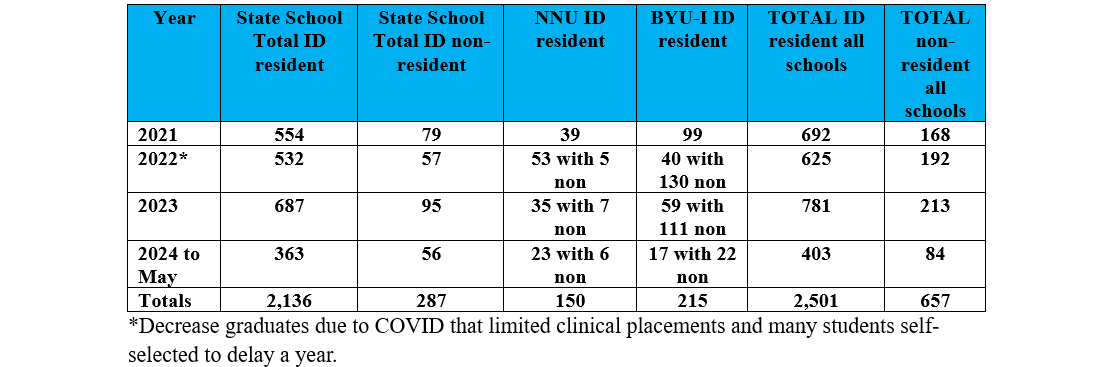
Education data shows that graduations have been consistent over the past two years. Most schools have plans to increase student enrollment but issues of faculty shortages, faculty salaries, no approved positions and issues with clinical experience placements pose barriers to having more students. To mitigate some of Idaho's nursing workforce needs, schools have focused on Idaho residents versus out of state admissions since 2021 and have reported these numbers.
Since 2021 there have been 2,501 Idaho residents who have graduated from Idaho schools of nursing. Schools have done well to address Idaho's nursing manpower needs, but sadly the increasing number of new graduates has not been able to meet the demands resulting from nurse retirements and population growth.
Idaho Resident and Non-resident RN Graduates 2021-May 2024
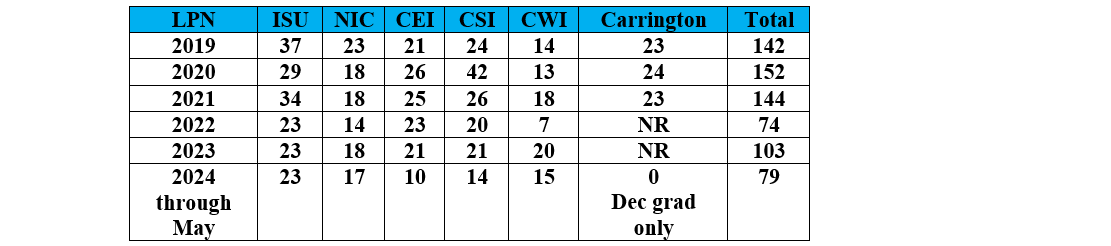
LPN nursing school graduations have been consistent with the exception of 2022 for the College of Western Idaho.
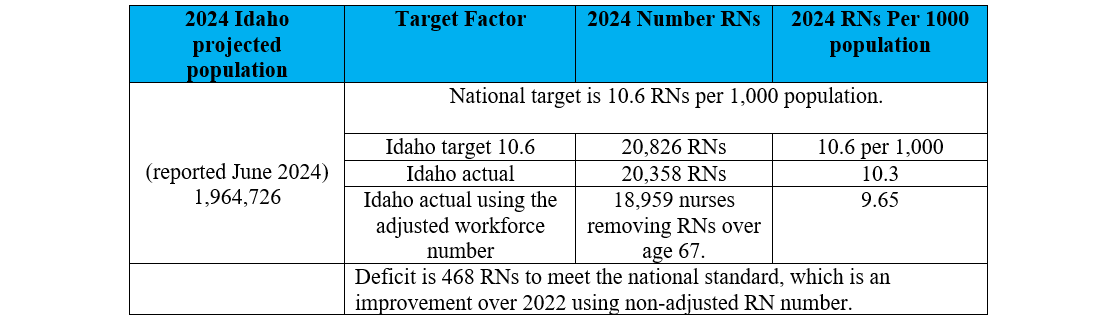
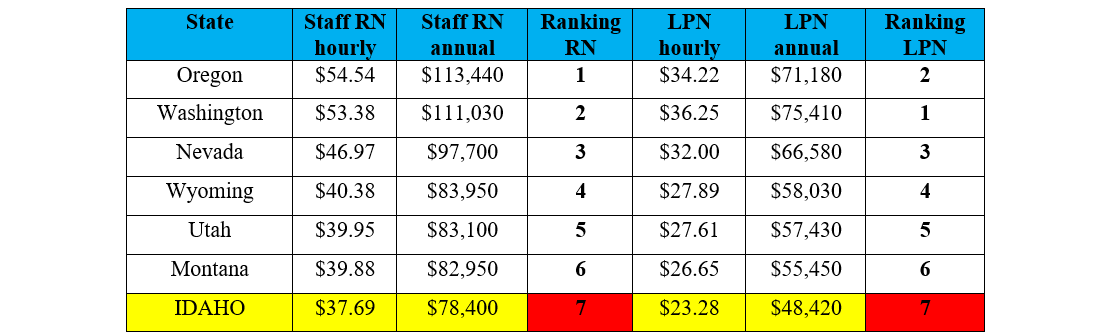
Job demand has been consistent. The Idaho Dept of Labor identified registered nurses as one of the highest demand jobs in the state in each of the past 4 years. The fundamental question is "how many nurses are needed?" There is a national target for this of 10.6 RNs per 1,000 population. Idaho has not met this standard in any year since data has been collected. There are many factors that impact this including, (1) limitations on schools because of faculty and clinical placements, (2) high retirement numbers from baby-boomer generation nurses that exceed new graduations, (3) Idaho's increasing population growth that has resulted from in-migration of adults versus birthrate which was the historical reason for population growth, and (4) nurse shortages in surrounding states that pay better with similar costs of living that attract nurses from Idaho to move.
2024 Idaho RN ratio per 1,000 Population
[source: U.S. Dept of Labor, Bureau of Labor Statistics; HRSA]
Hospitals across Idaho are still using travel agency nurse staffing services, but less than during the COVID years. Long Term Care and Assisted Living facilities across Idaho are using travel LPN and CNA staffing on a regular basis. The phenomena of solving staffing needs with travel nursing is not new, but it received increased national attention during the COVID staffing crisis. Much research on this is available. Essentially, there are fewer nurses doing travel nursing today than a few years ago and most are seeking placements in high salary states with good weather and good recreation. The novelty seems to have peaked and is now slowing. Additionally, study outcomes have failed to identify the relationships between quality of care impact and use of travel nurses (Aiken, Vander Weerdt).
Conclusion
The 2024 report discusses existing and future mitigation strategies that can impact the Idaho nursing workforce. Many of these have existed for the past several years and some have been implemented with measurable outcomes. Three things are certain. (1) Idaho will not stop the migration of adults into the state. It cannot control that many of these families will relocate their elderly parents to Idaho to be closer to family, and they will also need long term care or assisted living arrangements. (2) It will also be difficult to prevent the instate migration of nurses from rural towns to bigger towns or the Ada and Canyon counties because lifestyle opportunities, clinical experiences and other opportunities are greater, even if salaries are comparable. (3) Lastly, Idaho will not be able to meet its nurse staffing needs by relying on recruitment of nurses from other states to move to Idaho. There is no historical evidence that this has worked and competition in surrounding states continues to be attractive to Idaho nurses.
Using non-adjusted RN supply numbers that include retirement aged, licensed nurses, Idaho has a shortage of 468 RNs to meet baseline needs. Using adjusted numbers, excluding retirees, Idaho has a shortage of 1,867 RNs.
The best solution for Idaho to meet its nursing needs is to focus on the education of Idaho high school graduates to enter the nursing profession. To accomplish this, Idaho needs to focus on supporting the education programs to sustain workforce numbers.