Nursing continues to be a trusted profession. It is no surprise because we see nurses in different collaborative roles that effectively solidify teamwork and tirelessly promote lifelong learning. Over the years, nurses have entered uncharted workforce regions: advanced nurse practice, informatics, leadership, politics, and forensics, among others. Indeed, nursing can open a myriad of career opportunities, one of which is through specialty nursing practice. Specialty nursing carries an added responsibility and the privilege of being known as an expert in a particular nursing field. What does it take to be a board-certified operating room nurse? Or professional development practitioner? Or nurse executive?
Certification is a process by which agencies certify an individual licensed to practice a profession, like nursing, has met specific predetermined standards specified by that profession, including examination formulated by subject matter experts (Marfell et al., 2021). Certification positively affects patient care quality; for example, recent studies have shown significant associations between higher unit-level rates of specialty certification and lower rates of hospital-acquired infections, central-line-associated bloodstream infections, and ventilator-associated pneumonia (Smith et al., 2021).
The following board-certified nurses have shared some insights into their specialties. Their contributions inspire others to continue advancing the nursing profession. One such specialty and certification, the esteemed Nurse Executive (NE), is a testament to the dedication and expertise of those who hold it.
To earn the Nurse Executive (NE/NEA-BC) certification, one must have a Bachelor in Nursing (BSN) or a higher graduate degree. Verification of educational level must be submitted to the American Nurses Credentialing Center (ANCC) when first applying by sending copies of academic transcripts. The nurse must be an active and licensed registered nurse (RN) with at least 2000 hours of leadership, management, or administrative positions. Those positions must be of primary responsibility for the RN. The RN also must have at least 30 hours of continuing education (CE) credits in those areas within the former three years (Competency & Credentialing Institute, 2024a).
After paying the application fee and providing the evidence described above, the RN would take a certification exam for initial certification. For maintenance and recertification, the RN would have to apply, provide evidence of meeting requirements for recertification, and pay the fee. The NE/NEA-BC certification must be renewed every five years. The ANCC has a website where proof of meeting the maintenance requirements (i.e., CE hours, academic credits, publishing, presentations, preceptorships, and professional roles) is recorded. To renew, one must prove all the information listed for initial certification but have at least 75 hours of CE credits. There are eight other categories for renewal, and the RN must meet at least one of them. There are initial certification and renewal fees. The original application fee is $395 for non-American Nurses Association (ANA) members and $295 for ANA members. The renewal fee is $350 for non-ANA members and $250 for ANA members (Competency & Credentialing Institute, 2024a).
The Nurse Executive (NE) and Nurse Executive/ Nurse Executive NE/NEA-BC certification can work anywhere a position in nursing administration or nursing education is available. Generally, the nurse would be in an administrative position.
The NE-BC has allowed me to work in nursing and nursing education positions. It has not increased my salary per se. Still, it has allowed me to work in roles such as the interim Master of Science in Nursing (MSN) chair, program lead, course lead, and graduate nursing faculty in the Executive Leadership track.
I would say that the NE/NEA-BC certification is not one that most non-nursing health positions recognize as readily as having a Master in Business Administration (MBA). Still, part of that relies on the RN educating others as to the importance of this certification. It was worth the time and cost when I first sat for the exam after meeting the qualifications with my BSN. It gives one confidence that they have taken a competency-based exam verifying their knowledge and skills in leadership and management roles. It strengthens our profession as well. (Deborah Adelman, personal communication, September 2024)
Another nurse specialty/certification is the Certified Nurse in the Operating Room (CNOR). Eligibility requirements to sit for the CNOR certification include holding a current, unrestricted RN license; having a part-time or full-time job in perioperative nursing, administration, education, or research; having a minimum of two years and 2,400 hours of experience in perioperative nursing, with a minimum of 1,200 hours in the intraoperative setting within the past five years; and paying the initial cost of the certification exam of $445 (Competency & Credentialing Institute, 2024b).
The initial certification is valid for five years. After five years, the nurse must apply for renewal. One must complete 300 professional development activity points within the past five years to maintain certification. Some activities include academic study/teaching, continuing education, publishing, precepting/mentoring, participating in professional organization activities, and performing case studies. Other recertification eligibility requirements, in addition to having an active CNOR credential and current, unrestricted RN license, include working full—or part-time in perioperative nursing clinical practice, nursing education, administration, or research and have worked a minimum of 500 hours in perioperative nursing within the accrual period. Of those 500 hours, 250 must be in research, clinical practice education, or administration that impacts intraoperative patient care (Competency & Credentialing Institute, 2024b).
I have held the CNOR certification since 2005. This certification is held by over 40,000 nurses internationally. The nurse who obtains this certification demonstrates an ongoing commitment to the care of the surgical patient and dedication to perioperative excellence. The RN who holds a CNOR can work in any perioperative setting. This can be in hospital operating rooms, ambulatory surgery centers, sterile processing services (SPS), surgical clinics, or perioperative education. I have over 25 years of operating room experience and now have a role in providing professional development to operating room staff as a Nursing Professional Development Specialist.
There are many benefits to obtaining your CNOR certification. This strengthened my dedication and passion by validating my knowledge and skills while gaining well-deserved recognition for achieving nursing excellence in patient safety. Some studies identified a direct impact on patient care. There is a direct relationship between higher rates of nursing specialty certification and lower rates of hospital-acquired pressure injuries (HAPIs), patient falls, hospital-acquired infections (HAIs), and patient mortality (Boyle et al., 2014; Boyle, 2017). In addition, my related experiences opened doors for leadership opportunities. I am the current president of the Association of Perioperative Nurses (AORN) Graue Valley Chapter and a current member of the Chicago Association for Nursing Professional Development.
One of my proudest moments as a perioperative nurse was when I was awarded my certification. I had tangible validation of all my hard work in providing the best and safest care to my patients. My certification granted me the respect of my peers with the title of “role model.” It identified me as a resource person who wants to share knowledge, support team members, and drive to be a transformational leader. Be prideful in demonstrating your knowledge. This is a tangible way to demonstrate what a wonderful nurse you are! (Arlene Miranda, personal communication, September 2024)
Nurses can also specialize in working with patients with a physical disability or chronic illness—Rehabilitation Nursing certification (CRRN). If you are a nurse working with individuals with physical disability or chronic illnesses toward restoring, maintaining, and promoting optimal health, you are a rehabilitation nurse.
Eligibility for the initial CRRN exam includes a current, unrestricted US, US territories, or Canadian RN license and completion of at least one of the following at the time of application: two years of practice as an RN in rehabilitation nursing within the last five years; or one year of practice as an RN in rehabilitation nursing and one year of advanced study (beyond baccalaureate) in nursing within the last five years.
The exam is offered twice a year, during June and December. To register for the exam, you must submit a complete application with payment by the deadline on the website www.rehabnurse.org. The exam costs $300 for Association of Rehabilitation Nurses (ARN) members and $460 for nonmembers. Once you have passed the CRRN exam, the certification is valid for five years (Association of Rehab Nursing, 2024a).
To renew CRRN certification, you must meet the following requirements at the time of application: have a current, unrestricted RN license, complete 1000 hours of rehabilitation nursing experience within the five-year certification period, complete at least 60 points of credit that meet the published criteria within your five-year certification period (points of credit MUST be completed within the five-year certification period, not after selected for audit). There is a fee for CRRN renewal. Applications may be submitted beginning six months before the expiration date. The application deadline is the last day of the month, three months before expiration. Applications are accepted during the final three months, with a late fee (Association of Rehab Nursing, 2024c).
When you apply for certification, you will be asked to provide contact information from two professional colleagues who can verify your rehabilitation nursing experience. One must be your immediate supervisor or another CRRN. The second can be any other colleague, such as a nurse, physician, therapist, or social worker (Association of Rehab Nursing, 2024b).
CRRN nurses generally work in a general hospital with an acute rehabilitation unit, a long-term care facility, a home health agency, an insurance company, an outpatient clinic, an educational institution, a freestanding rehabilitation facility, or a private company.
I have determined that CRRN certification has many benefits. It demonstrates my knowledge and commitment to excellence in patient care and has helped me improve patient outcomes and satisfaction. In addition, my certification, and that of others, is a factor in the accreditation criteria by agencies and distinction by the ANCC Magnet Recognition Program, and it provides me with more excellent career opportunities.
I advise other nurses who are preparing for the CRRN to look at the test blueprint online. In addition to patient care, the test includes questions on legislation affecting rehabilitation and disability, reimbursement, ethics, case management, nursing theory, and nursing research. If you do not pass the first time, take the test at the next opportunity. (Jolene M. Simon, personal communication, September 2024)
Nursing Professional Development is yet another nursing specialty that offers certification. The Certified Nursing Professional Development Specialist (NPD-BC) works anywhere in the healthcare setting where staff education happens. This includes hospitals, clinics, long-term care facilities, nursing schools, government agencies, and public health offices, and research facilities. Nursing Professional Development Practitioners (NPDP) can be generalists (non-NPD-board certified) or specialists (NPD-BC). There is also advanced nursing professional practice certification (NPDA) (Harper et al., 2023).
To qualify for the NPD-BC certification exam, the nurse must hold a current, active RN license in a state or territory of the US or hold the professional, legally recognized equivalent in another country, hold a bachelor’s or higher degree in nursing (educational verification documents needed), have practiced the equivalent of two years full-time as a registered nurse, have a minimum of 2,000 hours of clinical practice in nursing professional development within the last three years, and have completed 30 hours of CE in nursing professional development within the last three years. The NPD-BC is active for five years when the nurse applies for renewal, meeting all the renewal requirements.
Earning the NPD-BC has many benefits for nurses. Being certified helped me improve my knowledge base and mastery of educational principles, increase my recognition and credibility by the system, leaders, and peers, and improve patient care.
Certification adds to knowledge and dedication to the profession and improves recognition and confidence. Note that the Competency & Credentialing Institute (CCI) offers a separate certification to advanced-practice NPD-BC nurses. (Beena Vallikalam, personal communication, September 2024)
The Certified Flexible Endoscope Reprocessor (CFER) is a nursing specialty that also offers certification. CFER-certified nurses work in hospitals, ambulatory surgery centers, clinics, medical device companies, and endoscopy offices. This certification is for the proper and safe processing and reprocessing of flexible endoscopes. This certification's requirements include completing 12 months of full-time employment or equivalent part-time hours processing flexible endoscopes. A manager must verify and sign this certification, and the signed document will be presented along with the examination application. This requirement can also be satisfied by completion of an Endoscopy Technician course with a minimum of eight hours and a grade of 70 percent or higher verified and signed by the instructor, and the signed document will be presented along with the examination application. If an applicant does not have any experience but working as a Sales Representative for GI/Endoscopy for at least 12 months, a verification of employment as such must be signed by the manager, and the signed document will be presented along with the examination application. The certification application fee is $128.00, valid for five years. A renewal fee of $125.00 is required, including 100 units of CE, which is comprised of college courses, chairing or serving on committees, or local and/or national level endoscopy organizations, certification test question reviewing, departmental in-service development and implementation, publishing endoscopic articles, and presentation of flexible endoscopic reprocessing educational programs.
One significant benefit of certification is the recognition of meeting measurable competency-based standards of the profession. It also ensures safe and effective levels of practice to protect the public. It also encourages continuing education and research for the specialty, promotes accountability, and upholds identified standards in this specialty. In addition, it enhances professional credibility, validates specialized knowledge, and signifies a commitment to lifelong learning. The CFER does not require a nursing board certification. However, my Operating Room (OR) experience and my other specialty certification (CNOR) have equipped me with the knowledge and confidence to do my job better and inspire others as they continue to excel in their OR skills. (Geri Weissmann, personal communication, September 2024)
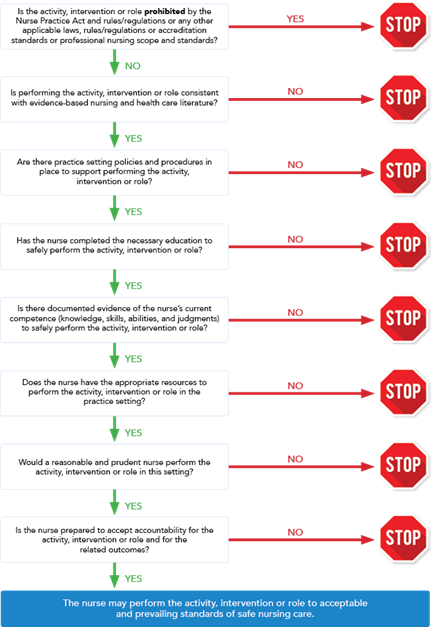
There are many other nursing specialties and certifications. This article introduces the reader to some nursing specialties and initial and renewal certification requirements. When nurses possess self-confidence because of validated expertise, it manifests in clinical judgment that leads to quicker execution of critical thinking abilities, ultimately resulting in safe patient care. Board-certified nurses reported feeling more empowered and in control of their practice. While it entails extra hard work and sacrifice, obtaining a specialty certification is well worth the effort for safe patient care and continuing professional development.