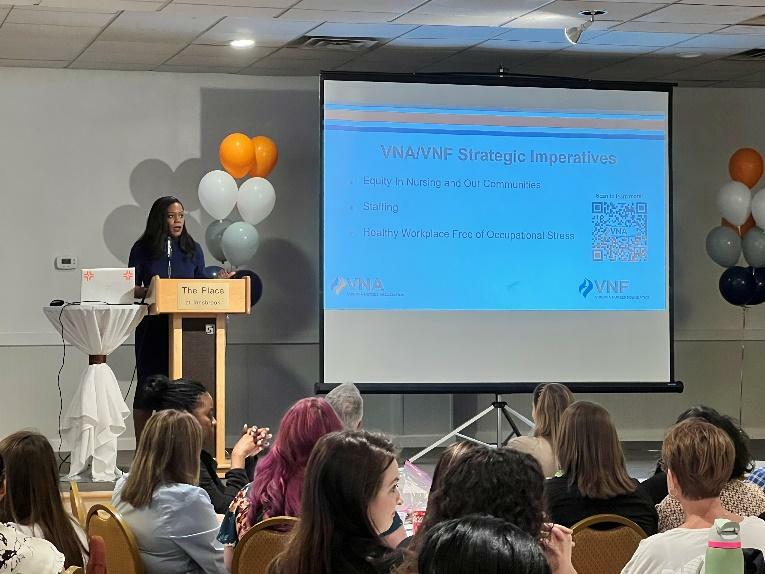
All Virginia nurses are invited to the Nurse Staffing Summit, hosted by the Virginia Nurses Association and Virginia Nurses Foundation on November 22-23, 2024. We’ll be addressing the pressing nursing staffing crisis in Virginia -- and across the country -- that has been top of mind for nurses everywhere. Top healthcare professionals, educators, and healthcare leaders will shape this conference by offering a comprehensive examination of the staffing challenges faced globally, nationally, and within the commonwealth. Participants can expect to take a deep dive into the multifaceted nature of this highly complex issue and gain insights into innovative strategies and actionable solutions that can be implemented across healthcare organizations in Virginia.
“Our healthcare system faces immense challenges. Cost-cutting decisions, an aging population, increased patient complexity and need, and an aging workforce all contribute to the current nurse staffing crisis that is negatively affecting nurses’ mental health and well-being,” said the American Nurses Association in an official statement. These same challenges negatively impact quality of care, and we must act now to create change in our systems to improve the health of our communities.
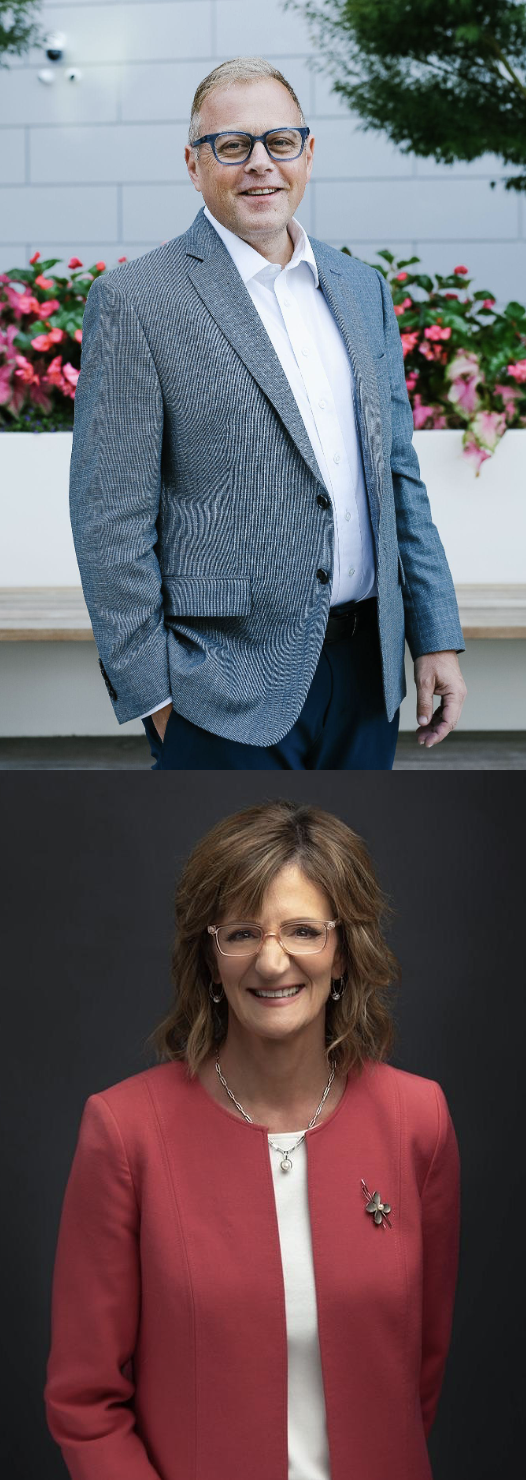
During the 2-day Nurse Staffing Summit, attendees can look forward to engaging keynotes that promise to inspire and equip participants with valuable insights and strategies. Renowned speakers such as Dennis McIntee (at left) from the Leadership Development Group will share his expertise on empowering nurses as leaders, while emphasizing the importance of emotional intelligence in enhancing leadership effectiveness and caregiving skills. McIntee's session will equip nurses with the tools to navigate challenges and foster a culture of leadership within healthcare settings.
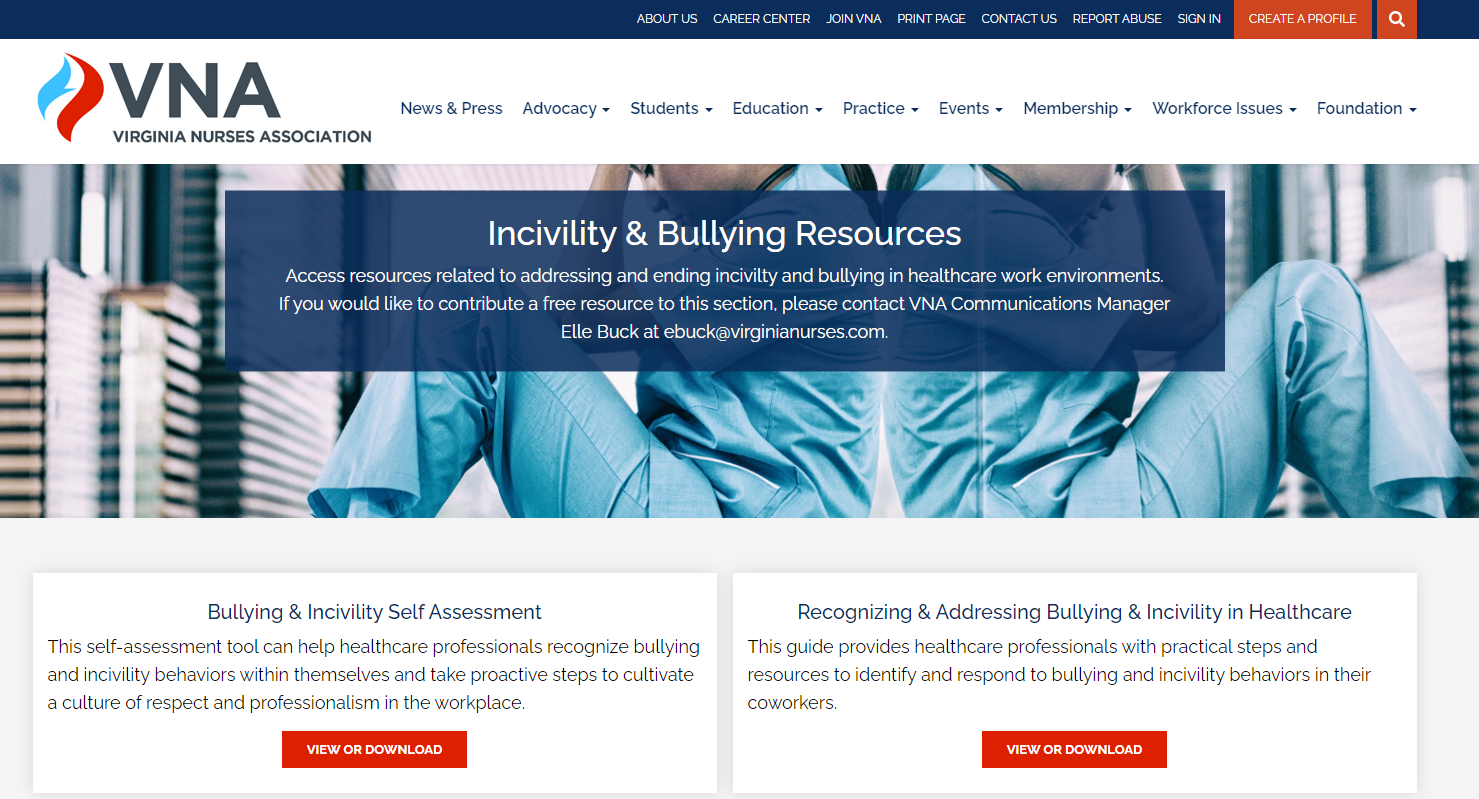
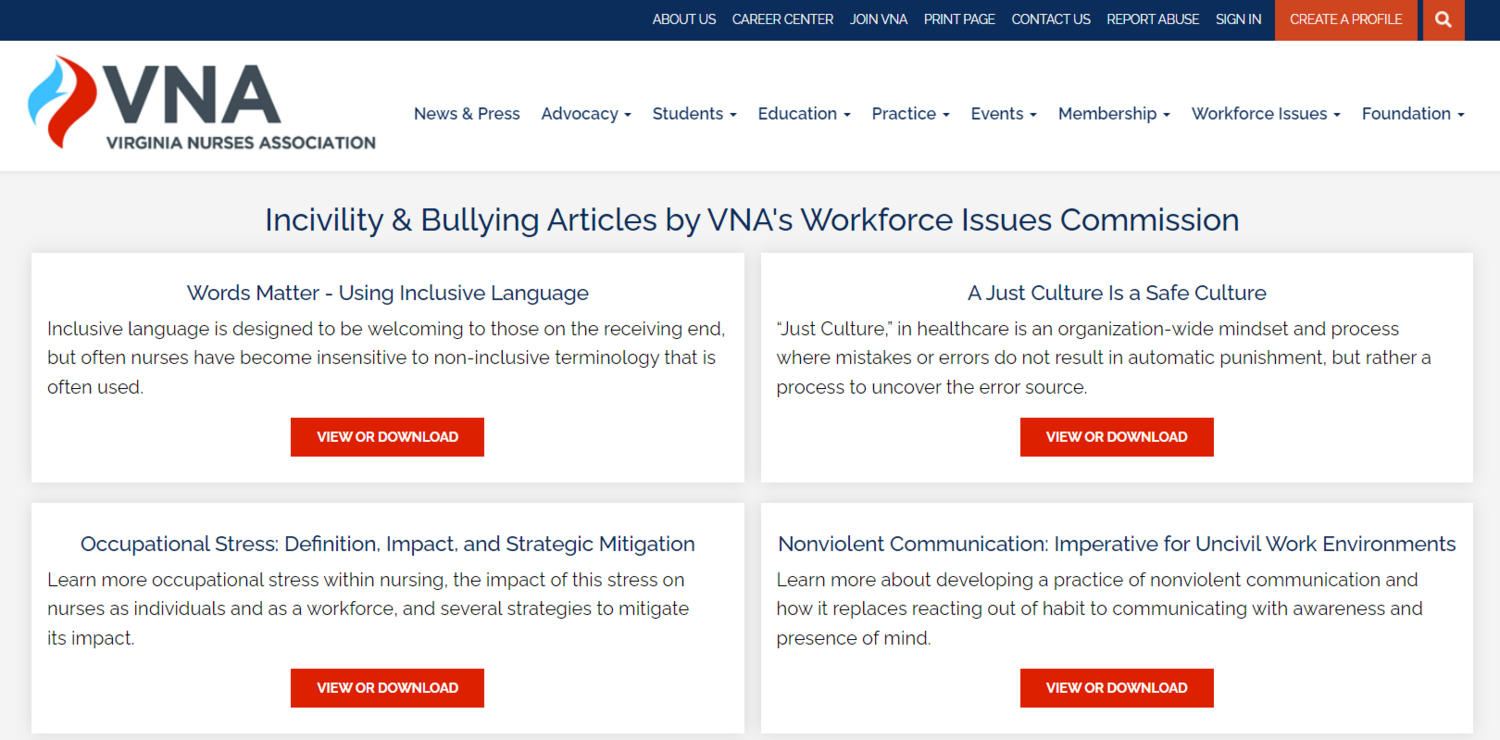
Additionally, Renee Thompson, DNP, RN, FAAN (at left) from the Healthy Workforce Institute will offer invaluable perspectives on creating healthy work environments that are conducive to nurse well-being and professional satisfaction. By addressing factors such as workplace incivility, bullying, and violence, Dr. Thompson's keynote will provide practical guidance for healthcare leaders striving to cultivate environments where every nurse feels valued and supported. These keynote sessions will serve as focal points for inspiring dialogue and actionable strategies aimed at fortifying the nursing workforce and improving patient outcomes in Virginia and beyond.
Throughout the summit, attendees will delve into the factors contributing to the staffing crisis, including the nursing education pathway, faculty shortages, retention, workplace culture, and challenges such as incivility, bullying, and workplace violence. Discussions will extend to examining the current reimbursement models for nursing and advocating for policy changes that can positively impact patient care and nursing practice. Moreover, the summit will highlight the role of technology in supporting nurses and alleviating their workload demands. With a focus on collaboration and networking, participants will have the opportunity to forge connections, share experiences, and cultivate solutions to effectively address the nursing staffing crisis. The accompanying exhibit hall will showcase organizations dedicated to supporting nursing, offering resources, innovations, and academic advancements aimed at bolstering the nursing workforce and enhancing patient care delivery in Virginia.
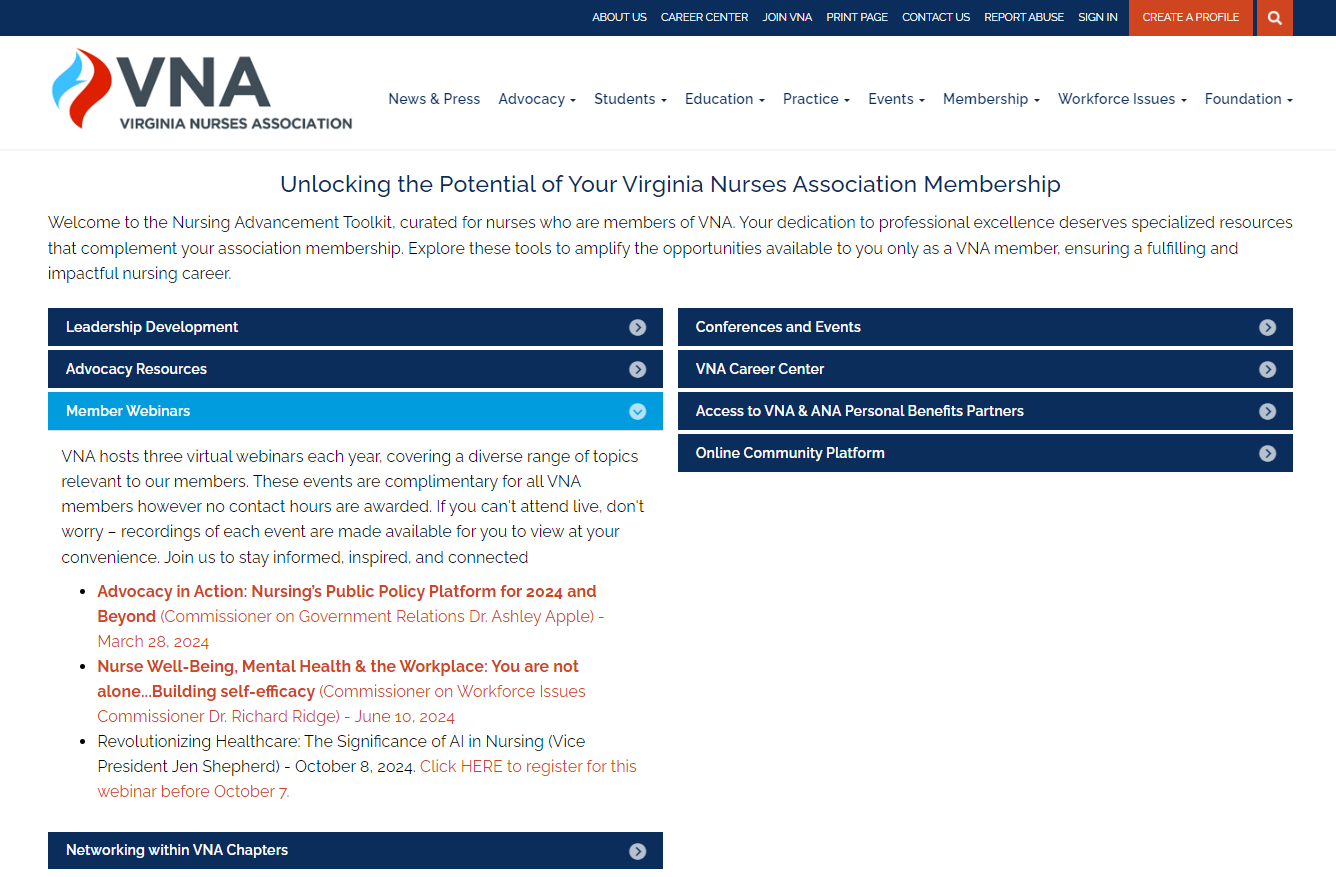
The 2024 Nurse Staffing Summit will be held at the Hilton Hotel & Spa in Short Pump, Virginia on November 22 and 23. This in-person summit has limited seating and registration is open now! Register today at the price of $300 for VNA members and $389 for nonmembers. Not a VNA member? You can join VNA and ANA today for just $15 a month and save nearly $200 in conference registrations! Join the movement for safe staffing. We hope to see you this November!




























 In June, the American Nurses Association released their first guidelines on
In June, the American Nurses Association released their first guidelines on 
 Kudos to Immediate Past VNA President Dr. Linda Shepherd, DPN, MBA, RN, NEA-BC (at left) for her contributions to
Kudos to Immediate Past VNA President Dr. Linda Shepherd, DPN, MBA, RN, NEA-BC (at left) for her contributions to  This acclaimed workbook delivers an organized, systematic roadmap for the development, implementation, evaluation, and completion of the DNP Project. Designed by two nurse educators motivated by their own frustrating DNP experiences to help the next generation of students, it consists of a collection of lessons guiding readers, step-by-step, through the entire DNP Project process. Anchored in a real-world context with more than 100 learning activities, the resource promotes active learning and delivers practical tips and advice for every stage of the project
This acclaimed workbook delivers an organized, systematic roadmap for the development, implementation, evaluation, and completion of the DNP Project. Designed by two nurse educators motivated by their own frustrating DNP experiences to help the next generation of students, it consists of a collection of lessons guiding readers, step-by-step, through the entire DNP Project process. Anchored in a real-world context with more than 100 learning activities, the resource promotes active learning and delivers practical tips and advice for every stage of the project

 Looking ahead: imagining ANA in 2040
Looking ahead: imagining ANA in 2040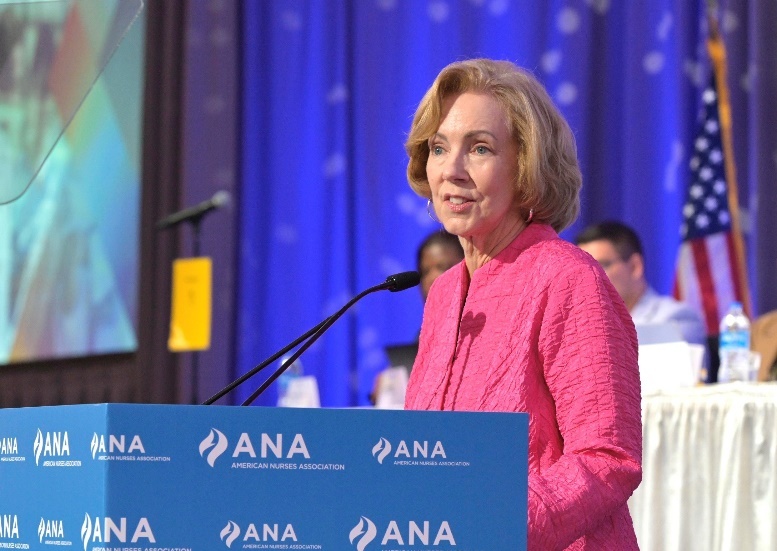 In her report to the Assembly, ANA Enterprise CNO Debbie Hatmaker, PhD, RN, FAAN, thanked members for coming together to demonstrate "the power of nurses."
In her report to the Assembly, ANA Enterprise CNO Debbie Hatmaker, PhD, RN, FAAN, thanked members for coming together to demonstrate "the power of nurses."