Nurse Staffing
Staffing to Standards
Organizations partially comply with national and regional standards, such as ICU (1:2) and ER (1:3 or 1:4) ratios, but struggle to adhere to them in med-surg and telemetry units. Staffing often depends on census rather than patient acuity, leading to inconsistencies. Deviations frequently result in high nurse-to-patient ratios, particularly in med-surg and behavioral health units, where standards are less enforceable.
Challenges include chronic understaffing, overwork, burnout, and retention issues driven by high workloads and lack of support. Some facilities provide extra staff during peak times, but others fail to replace absent team members.
Improvement recommendations emphasize a shift towards acuity-based staffing, enhanced retention strategies through better work conditions and pay, increased auxiliary support, and established mechanisms to ensure consistent standard adherence.
Overtime Management
Handling overtime, on-call time, and canceled shifts varies across facilities. Overtime is generally offered as a voluntary option, incentivized with bonuses or higher pay rates, though some facilities have mandatory schedules. Overtime compensation varies, with facilities often trying to avoid it by redistributing workloads. Challenges include feelings of pressure to work extra shifts and the potential cancellation of overtime if census levels drop. On-call time may be mandatory or voluntary, with minimal pay leading to dissatisfaction. Staff are expected to be available within a specific time frame, often used to cover unexpected gaps. Canceled shifts are communicated through various methods with varying notice periods, and a rotation system is commonly used to decide whose shift will be canceled next. Staff often need to use PTO for compensation, leading to frustration. Challenges include perceived inequities, impact on workloads, and poor management of on-call and overtime systems. Positive practices include flexible scheduling, significant bonuses, equitable rotation systems, and clear communication, which staff appreciate.
Census Fluctuations
Common responses to low census include sending staff home, often requiring the use of PTO to maintain pay, or seeking volunteers before mandating early departures. Some facilities implement flexing off in blocks. Nurses may be floated to other units with staffing shortages, and some facilities maintain core staffing in unpredictable units like ED and L&D. During high census periods, facilities often overburden existing staff by increasing nurse-to-patient ratios, call-in on-call staff or offering incentives for additional shifts. Adjusting assignments, such as reassigning patients or using charge nurses and float nurses, is also common. Challenges in managing census fluctuations include inconsistent practices, impact on staff morale, and short-term solutions that fail to address root causes. Positive practices involve flexibility in staffing models, proactive capacity management, and effective teamwork and communication, with facilities reporting better outcomes when using well-developed flex pools or PRN staff and employing task-based roles or virtual nursing during high census periods.
The survey highlights varying practices in how healthcare facilities handle staffing fluctuations due to patient discharges, transfers, or admissions, revealing differences in efficiency and organization. Some facilities adjust by sending nurses home, putting them on call, or using float pools, agency nurses, or flex pools to manage staffing gaps. Others rely on charge nurses to rebalance workloads or involve administrative staff in patient care. Incentives like bonus pay or gift cards are sometimes offered, while productivity grids or rotation systems guide staffing decisions in certain facilities. However, some responses depict chaotic or poorly managed systems, with inconsistent protocols, understaffing, and prioritization of financial gain over safety. Inadequate adjustments, such as not recalling staff when census increases or continuing admissions despite insufficient staffing, exacerbate challenges. A few facilities demonstrate efficient strategies, such as central staffing hubs and team-based approaches, while others lack clear protocols, handling fluctuations on a case-by-case basis.
Alternative Models
Facilities employ various alternative staffing models to address workforce needs, including using agency and contract nurses, in-house agency nurses, and offering higher-paying in-house contracts to existing staff. Float pools or flex pools, PRN staff, and dynamic nursing models where multiple nurses collaborate are common. Support roles such as CNAs, LPNs, PCTs, paramedics, and pharmacists for medication administration and supplement nursing staff. Virtual nursing models are used for tasks like admissions and documentation. Specialized roles and team-based models, such as team nursing with RNs, LPNs, and CNAs working in pods, are also implemented. However, challenges include insufficient training for float or agency nurses, uneven workload distribution, retention and recruitment issues, and inconsistencies in support roles. Positive practices include team and pod-based approaches, flexible scheduling, resource optimization, and overstaffing during peak census periods to offer flexibility and alleviate workloads. These strategies aim to provide effective staffing solutions while addressing unit-specific needs and ensuring nursing satisfaction.
Recruitment and Retention
Retention strategies for nurses encompass a range of monetary incentives, career development opportunities, benefits, and workplace environment improvements. Facilities often provide retention bonuses, pay raises, sign-on bonuses, incentive pay for extra shifts, and cost-of-living adjustments to retain staff. Career development opportunities include clinical ladder programs, education support such as tuition reimbursement and scholarships, and residency programs for new graduates. Comprehensive benefits packages offer competitive retirement plans, generous PTO, and full medical insurance, often including dependents. Recognition and appreciation come through gifts during special weeks, staff appreciation events, and healthcare service discounts.
Flexible scheduling, improved staffing ratios, open communication, and employee engagement committees enhance the workplace environment. Challenges include a focus on recruitment over retention, inadequate raises, and low morale due to a perceived lack of appreciation and poor management communication. Notable successes involve longevity incentives, fostering a healthy work culture with positive recognition and team-building activities, and retention interviews to proactively address staff concerns. These strategies create a supportive and rewarding work environment, ultimately promoting nurse retention.
Education, Training, and Development
Onboarding and Orientation
A nurse's preparedness to enter the workforce varies widely based on several factors. Positive experiences include comprehensive orientation programs with dedicated preceptors, effective mentorship, hands-on experience in nursing school, and supportive work environments. These factors significantly contribute to nurses feeling well-prepared. On the other hand, negative experiences often stem from inadequate orientation or training, lack of clinical preparation in nursing school, overwhelming first experiences, and staffing or resource issues. Recurring themes highlight gaps in nursing school education, the importance of well-structured and lengthy orientation programs, the critical role of skilled preceptors, and the benefits of supportive work environments. Adequate preparation involves thorough, hands-on training and robust support systems to ease the transition into professional practice.
Orientation practices in nursing typically involve structured programs that combine classroom training and preceptorship, often lasting between 6-12 weeks, with new graduates sometimes receiving up to 12-16 weeks of orientation through residency programs or structured onboarding. Preceptorship is a common approach, pairing new nurses with experienced preceptors and providing resources like checklists to guide the process. General hospital orientation is followed by unit-specific training to introduce workflows and patient care expectations. Shadowing experienced nurses is often used during the initial phase of orientation. Specialized units like critical care, OR, and ER have extended, more intensive orientations, and residency programs may provide ongoing education and peer support.
The findings on individualizing orientation in nursing highlight several common practices. Orientation programs are often tailored to the nurse's prior experience, skill level, and comfort, with more experienced nurses sometimes receiving a fast-tracked program. Preceptors are key in customizing the orientation process and assessing strengths and weaknesses to provide targeted support. The duration of orientation is flexible, extending based on individual progress and feedback, and often focuses on specific clinical skills relevant to the new role. A one-on-one approach with preceptors allows for personalized learning and daily feedback.
However, challenges include the initial reliance on standardized components, which can limit flexibility, and resource constraints that affect the quality of individualized training. Inconsistencies in orientation practices across different units also pose a challenge. Best practices identified include regular feedback and adjustments to orientation plans, using skill-specific and goal-oriented checklists, and maintaining flexibility in the duration of the orientation to accommodate individual learning curves. These strategies help ensure that orientation programs effectively meet the unique needs of each nurse.
Changing Skill Level
When changing skill levels, common orientation processes typically involve a preceptor-led approach, where nurses are paired with a preceptor for a duration that varies based on the unit's complexity and the nurse's experience. Unit-specific orientations are tailored to the new unit's policies, workflows, and technologies. At the same time, transfers generally receive shorter orientations than new hires unless they move to a significantly different specialty.
Challenges in these practices include inconsistent orientation durations, a lack of standardized protocols, and staffing shortages that limit the ability to provide comprehensive training. Best practices for improving orientation involve flexible and individualized programs tailored to the nurse's experience and comfort level, consistent preceptorship with assigned preceptors, and supportive transition models offering mentorship and extended orientation for specialty units. These strategies help enhance the effectiveness and satisfaction of orientation processes.
Evaluation Practices
Evaluation practices of orientation in nursing involve several key methods. Formal evaluations are commonly structured and conducted by preceptors, managers, or educators, with specific timelines such as 30, 60, and 90-day assessments. Skills checklists and task lists signed off by preceptors or managers are frequently used to evaluate competencies. Feedback mechanisms, including surveys and interviews, are incorporated to gather input from orientees and preceptors, and managers or clinical educators often oversee the evaluation process. Challenges in orientation evaluation include inconsistent implementation across units, superficial or minimal assessments, and limited opportunities for orientees to provide feedback. Best practices identified include comprehensive and regular evaluations with clear timelines, inclusive feedback mechanisms that collect input from orientees and preceptors, and a focus on competencies and readiness for independent work, ensuring thorough and actionable insights into the orientation process.
Career Development and Advancement
Career advancement opportunities in nursing include clinical ladder programs, leadership and management roles, education and certification support, promotions, recognition programs, and specialized roles. Clinical ladder programs provide structured pathways for career progression with benefits like pay increases and professional development. There are also opportunities to advance into charge nurse, supervisor, or manager positions, often supported by leadership development and mentorship programs. Tuition reimbursement and financial incentives help nurses further their education and obtain certifications. Internal promotion policies highlight roles in administration, education, and specialized nursing. Recognition programs like Daisy Awards and peer-recognition initiatives value staff contributions. Additionally, nurses can transition into specialized roles like quality assurance or infection control, with some organizations supporting career exploration through shadowing programs.
Challenges include perceptions of inequity, difficulty accessing programs, limited scope in smaller facilities, the conflict between retention and career advancement, and inadequate recognition. Staff often feel opportunities are based on favoritism and that clinical ladder programs are hard to achieve due to documentation requirements. Smaller facilities may offer limited advancement options, and while valued, career advancement can contribute to losing bedside nurses. Recognition programs are sometimes seen as insincere or tokenistic.
Innovative practices involve well-supported clinical ladder programs with financial incentives and mentorship, education support through tuition reimbursement and partnerships, leadership development tracks with mentorship, and recognition programs with tangible rewards like bonuses and pay increases. These practices help motivate and satisfy staff, contributing to effective career advancement.
Professional Development
Professional development opportunities are abundant, such as tuition reimbursement, clinical ladder programs, certification incentives, and in-service and online learning. Many facilities support advanced degrees and certifications through tuition reimbursement programs, offering financial assistance to help employees further their education. Clinical ladder programs provide structured paths for career advancement and recognition, encouraging participation through leadership opportunities and committee involvement. Additionally, facilities often incentivize specialty certifications by offering financial bonuses or covering certification costs. Continuous education is supported through regular skills fairs, in-services, and online modules, ensuring employees stay updated on necessary skills and knowledge.
However, challenges persist in accessing these opportunities. Limited awareness or underutilization of available programs is a common issue, with many nurses unaware of the resources at their disposal. Resource and time constraints, particularly staffing shortages, hinder the ability to complete educational requirements. Moreover, some staff perceive programs like clinical ladders as providing minimal incentives, leading to low engagement. Despite these obstacles, best practices can enhance participation by ensuring accessible financial support, offering flexible learning opportunities, and fostering mentorship and leadership development. Clear tuition reimbursement processes and certification funding encourage staff to pursue advanced education, while online and in-person learning options accommodate different schedules. Mentorship programs and leadership training are vital for professional growth, helping to build a robust support network for career advancement.
Policy and Advocacy
Nurses access information from various sources, including state boards of nursing through emails, newsletters, publications, professional organizations such as ANA and LSNA, social media platforms and online resources, news and media outlets, workplace communications, and self-initiated research. However, they face challenges such as inconsistent or insufficient communication, being too busy to keep up with updates, limited awareness of available resources, dependence on word-of-mouth, and a perceived focus on organizational priorities over nurse advocacy. Recurring themes highlight the importance of professional organizations as key advocates, time and accessibility challenges, and the crucial role of employers in disseminating information. Suggestions for improvement include enhancing employer communication, promoting professional memberships, developing user-friendly information platforms, offering education and advocacy training, and ensuring streamlined updates from state boards. These steps can help nurses stay informed and effectively navigate legislative changes.
Communication with Leadership
Organizations use various mechanisms to facilitate communication between nurses and leadership. Formal channels include surveys, regular meetings, committees, councils, and online reporting systems. Informal channels feature open-door policies, emails, and leader rounding. However, challenges persist, such as perceived lack of action on feedback, fear of retaliation, tokenistic initiatives, dismissive leadership attitudes, lack of transparency, and time constraints. Recurring themes include a disconnect between leadership and bedside nurses, unionization efforts due to dissatisfaction, and the emotional toll of feeling ignored. Effective communication relies on transparency, clear follow-up, and actionable outcomes. Suggestions for improvement include establishing accountability for feedback, ensuring anonymity and safety, increasing proactive leadership engagement, empowering nurses through shared governance, designing action-oriented surveys, and providing education and advocacy training. These steps can help bridge the gap between frontline staff and leadership, fostering a more inclusive and responsive environment.
Conclusion
In conclusion, the Nursing Workforce Effectiveness Initiative has illuminated critical insights into the challenges and opportunities the nursing workforce faces. The findings from the staff nurse survey emphasize the importance of addressing staffing standards, improving retention strategies, enhancing professional development, and fostering effective communication with leadership. While notable examples of innovative practices and effective solutions exist, many facilities still face significant hurdles in creating sustainable and supportive work environments. Organizations can strengthen workforce capacity and improve nurse satisfaction and patient outcomes by prioritizing actionable feedback, promoting transparency, and investing in education and advocacy. These collective efforts will be instrumental in advancing the nursing profession and ensuring high-quality care delivery.
Next Steps
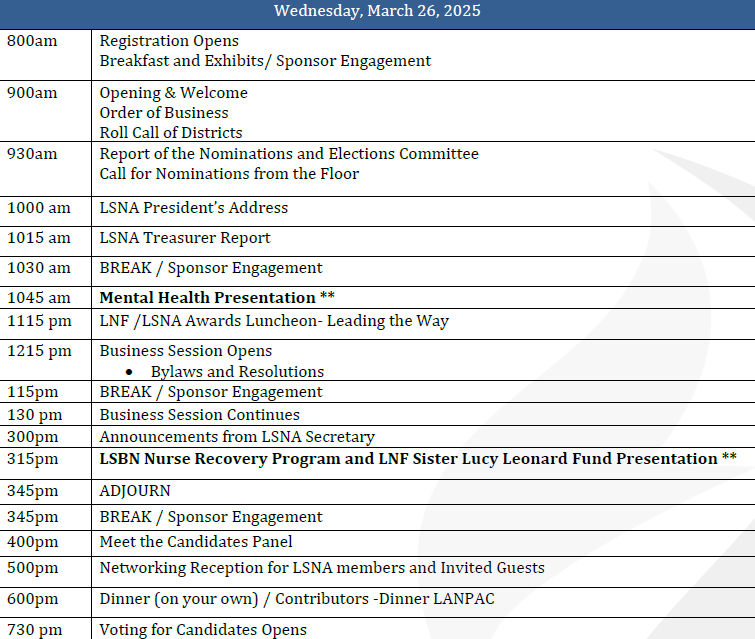
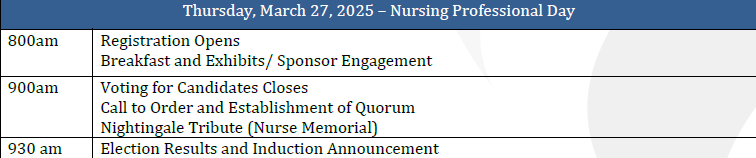
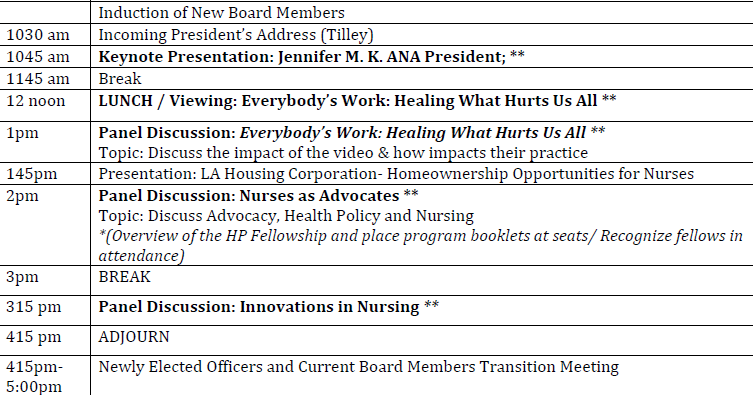
Q1 2025: Present findings to LSNA Board, initiate pilot programs, begin legislative advocacy efforts, and establish evaluation metrics.
Q2 2025: Launch mentorship and residency programs; develop and implement flexible staffing strategies.
Q3 2025: Assess progress and prepare recommendations for 2025 initiatives.