The Virginia Nurses Association and Virginia Nurses Foundation are hosting the Nurse Staffing Summit on November 22-23 at the Hilton Hotel & Spa in Short Pump, Virginia. As the healthcare industry confronts an unprecedented staffing crisis, this event will serve as a vital platform for addressing challenges and exploring innovative solutions. Healthcare professionals, educators, policymakers, and industry leaders will come together to examine the complexities of the crisis and strategize on strengthening the nursing workforce for the future.
This summit is packed with dynamic presentations and interactive sessions, focused on the critical issues impacting nurse staffing in Virginia and beyond. Topics will include the nursing shortage and its causes—such as educational barriers, retention challenges, workplace culture, and reimbursement models—as well as the influence of technology and policy on the profession’s future.
Keynote Speakers
The summit will highlight two influential speakers who are leaders in the field:


Dr. Katie Boston-Leary, PHD, MBA, MHA, RN, NEA-BC, FADLN, will deliver her keynote Sustainable Staffing Solutions in Nursing, and discuss how the nurse staffing shortage continues to impact nurses, patient care and population health. The time is now to implement solutions using a ”tribrid” approach, strategic partnering and human centered thinking to build healthy work environments for optimal outcomes to be attained for nurses and patients. It is high time to create a world where nurses are practicing in an ideal caring environment and patients feel valued and optimally cared for.
Summit Highlights
In addition to the keynote addresses, the summit will feature:
-
A Leadership Intensive by Dennis McIntee, CEO & Co-Founder of the Leadership Development Group, focusing on transformative leadership skills for nurses.
-
The Nurse Leadership Academy Rapid Fire Series, showcasing cutting-edge leadership projects by VNF Fellows, delivered in an engaging, fast-paced format.
-
Work Environment Spotlight: Cultivating a Healthy Work Culture: Strategies to Eradicate Workplace Bullying and Incivility, led by Renee Thompson, DNP, RN, FAAN, CSP, of the Healthy Workforce Institute. Dr. Thompson will explore practical tools and strategies participants can immediately implement to address bullying and incivility within the care environment. When nurses are equipped to address disruptive behaviors, employees stay, and patients achieve better outcomes.
-
Film Screening of “Everybody’s Work: Healing What Hurts Us All”, a documentary examining the pervasive issue of racism in healthcare. A Fireside Chat will follow with keynote speaker and film participant Dr. Katie Boston-Leary, allowing attendees to engage in discussions on how systemic racism affects both patients and nurses, with reflections from healthcare leaders.
- Rapid-Fire Podium Presentations featuring Virginia clinicians sharing practical solutions on staffing, workforce development, and building equitable workplace environments.
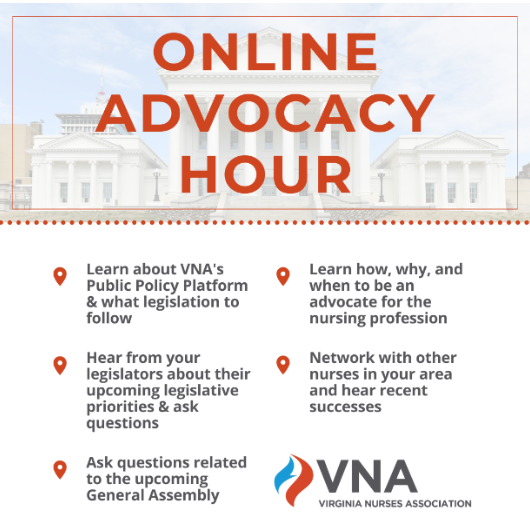
Advocacy and Networking Opportunities
The summit will also offer an in-depth panel discussion on strengthening nurse staffing in Virginia, featuring leaders from VNA and healthcare organizations across Virginia. Attendees will learn about ongoing advocacy efforts, best practices, and successes in implementing nurse staffing committees. This is a unique opportunity for healthcare professionals to engage with thought leaders and collaborate on strategies to address the staffing crisis.
With 12.5 nursing contact hours available and an exhibit hall showcasing the latest resources and innovations for nursing, the summit promises to be an empowering experience for all attendees.
Registration Information
Registration for the event is open until November 14 at 5 PM. VNA members receive a discounted rate of $300, while nonmembers can register for $389. Register online via the Nurse Staffing Summit website and take advantage of membership opportunities with VNA and the American Nurses Association to save on registration!
This summit is a must-attend for healthcare professionals looking to navigate the staffing crisis, improve workplace culture, and drive meaningful change in the nursing profession. We hope to see you there!